Unveiling the Enigmas of Radicular Cysts: A New Perspective on Their Development and Progression
Abstract
Introduction: Radicular cysts can therefore be described as the most frequently encountered inflammatory odontogenic cysts which arise in response to infection and inflammation of the tooth. Nonetheless, they still rank among the most obscure concepts in oncology and as far as the particular mechanisms that congenital oncology as well as its development are concerned, these matters are still very much a topic of conjecture. It therefore follows that this study wishes to offer a new milestone of how these pathophysiological entities affects cyst formation within the radicular context given the varying inflammatory/immune markers assessments.
Materials and Methods: This case-control study included 100 participants, divided into two groups: pa control group with
f
ifty study subjects and the second group of study subjects with radicular cysts n= 50. The following biomarkers were tested:
Interleukins 1 (IL-1), interleukins 6 (IL-6), tumour necrosis factors-α (TNF-α), matrix metalloproteinase 1 (MMP-1), matrix
metalloproteinase 9 (MMP-9), lipopolysaccharide (LPS), soluble receptor activator of nuclear factor kappa-B ligand (sRANKL).
Certain physical and biochemical variables such as white blood cell count, haemoglobin, neutrophil, age, weight index, systolic
blood pressure and diastolic blood pressure were also considered. Inferential data was tested using t-test of two samples and
compared the results against a set p-value of < 0.05.
Results: In comparison to the control
group, the subject group was
of similar
weight age, SBP, DBP and
or haemoglobin.
However, results got some changes in
the pro and anti-inflammatory cytokines such as IL-1, IL-6, TNF-α,
MMP-1, MMP-9 and LPS, sRANKL, neutrophils
were found significant with p value of 0.015, 0.024, 0.0.31, 0.004, 0.017,
0.033 respectively.
![]() Conclusion: In the case of radicular cysts, some of these factors have been highlighted, such as inflammatory cytokines, matrix metalloproteinases and a part of immune
response. Relatively higher
levels of pro-inflammatory cytokine such as IL-1, IL-6, TNF-α and MMP-3 observed
in the subjects suggest inflammatory and remodelling based
concept of cyst development. From these findings it will possible to do more that may enable the researcher to come up with even more refined intervention measures
to control radicular cysts.
Conclusion: In the case of radicular cysts, some of these factors have been highlighted, such as inflammatory cytokines, matrix metalloproteinases and a part of immune
response. Relatively higher
levels of pro-inflammatory cytokine such as IL-1, IL-6, TNF-α and MMP-3 observed
in the subjects suggest inflammatory and remodelling based
concept of cyst development. From these findings it will possible to do more that may enable the researcher to come up with even more refined intervention measures
to control radicular cysts.
1. Introduction
Radicular cyst is a cyst of jaw which originates from
rest of Malassez present in the periodontal ligament due to
inflammatory process after pulp death. Radicular cyst is the most
common odontogenic cyst having frequency of 52% to 68% of
all the cysts affecting the jaws1. The prevalence of radicular cyst
is highest in third decade of life and is more common in men
than women. They are more common in maxilla than mandible.
Usually, it is a symptom less lesion of jaw but sometimes may
grow slowly and represents as a symptomatic swelling visible in
oral cavity2. On radiograph, the radicular cyst usually appears as
an oval or pear shaped unilocular radiolucency around the apex
of non-vital tooth and sometimes around the lateral side of root3.
It is very difficult to distinguish the radicular cyst from periapical
granuloma on the basis of radiograph alone but if the radiolucent
area is greater than 2cm then it may be more likely a cyst4.
Histologically, the radicular cyst is lined by stratified squamous
epithelium which is derived from odontogenic epithelium called
rest of Malassez. Radicular cyst is usually present at the apex
of tooth which has become on vital after caries, pulp necrosis
or physical injury5. It is named as apical, lateral or residual
radicular cyst depending on the position of cyst in association
with the involved tooth: apical radicular cyst is located around
the apex of involved tooth; lateral radicular cyst is present on
the lateral side of involved tooth and residual cyst develops in
the jaw even after the extraction of offending tooth6,7. Usually
radicular cyst develops within untreated chronic periapical
granuloma but all granulomas do not proceed to radicular cyst.
Mostly they are associated with permanent dentition and are
rarely seen in deciduous teeth (Figure 1).
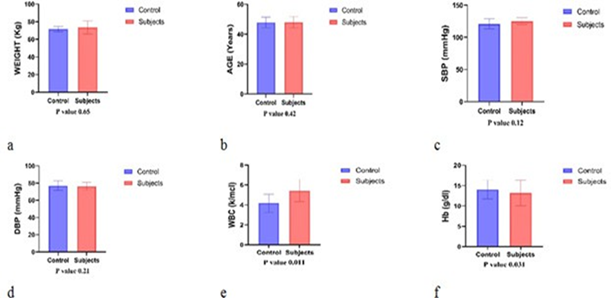
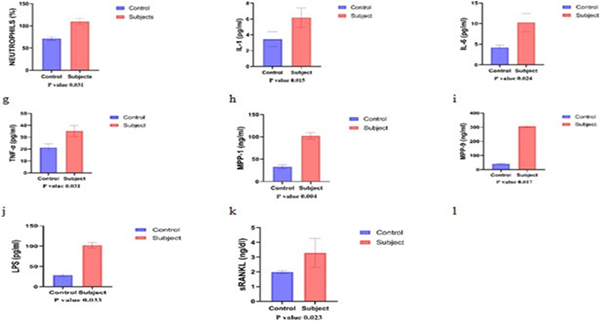
Figure 1: Role of different variables of medical
importance and their potential role in the development of radicular
cyst.
Initially, the oral microflora enters the tooth
pulp through carious
cavity but due to the local environment of root canals
the gram- negative anaerobic
microorganisms become predominant8.
At a later stage, the infected pulp becomes polymicrobial community and has several pathogenic and biological properties. These microorganisms may cause mitogenic
activity, antigenicity, enzymatic breakdown, chemotaxis and host
defence activation9. The
microorganisms present in the root canal system advance towards periapex releasing
their products (endotoxin) and triggers the various host defence reactions
consisting of activation of several
1. Materials and Methods
Fifty
male patients with diagnosed radicular cyst (RC) associated with root canal
failure teeth were enrolled for the present study from the period of September
2013 to November 2015. The normal pulp tissue of fifty healthy teeth extracted for orthodontic treatment served as
control. Informed consent was taken from the entire participants of the study.
Patients having history of antibiotic therapy in past three months or having
diseases that interfere with periodontal status such as liver disease,
hypertension, diabetes etc. and smokers were excluded from this study. Tissue homogenates of radicular cyst and normal pulp
were prepared and stored at -70°C for the assessment of different biochemical
variables. All the protocols
performed in this study were approved by research ethical committee School of
Pain and Regenerative Medicine (SPRM), The
University of Lahore.
1.1. Analytical assays
Different
biochemical assays were performed through their specific protocols.
Lipopolysaccharides (LPS) were measured through spectrophotometer. Whereas, soluble
receptor activator of nuclear
factor Kappa-β ligand (sRANKL), interleukins (ILs) and matrix
metalloproteinases (MMPs) were measured through commercially available ELISA kit methods
provided by Abcam S’ and Enzo Laboratories.
1.2. Statistical analysis
Independent
samples t-test was also used to test the hypothesis where control group comprised 50 subjects and the subject group comprised 50
subjects. This parametric test was conducted to test hypotheses that exist as
to whether the differences in the mean inflammatory markers and protein
expressions in the groups were significant. The cut off point for significance was set at 0.05. Descriptive statistics were evaluated
by SPSS software, version 25 and the p-value of less than 0.05 was
considered biomechanical significant.
2. Results
Several
clinical and biochemical markers were compared between the Control group
which consisted of fifty subjects
and the subject group of fifty
subjects suffering from radicular cysts. The analysis of variance
indicated nonsignificant p values for
weight: For the number of PVCs, the F statistic was F (1,168) = 0.659; for age, F (1,168) = 0.426; SBP F (1,168) = 0.124; DBP
F
(1,168) = 0.216; and Hb F (1,168) = 0.256. However, in the case of several
markers, the difference was revealed out to be significant between the subject
group and control group. In the present study, there was a significant raise in
the mean count of
WBC at 5.44 ± 1.11 k/mcl in the patients of
radicular cyst compared to the control group with the mean count of 4.18 ± 0.912 k/mcl with p-value 0.011.
The subject group also showed
a higher neutrophil % 109.88 ±
6.88% as compared
to the control group with mean 71.59 ±
4.29, p = 0.031. Regarding
acute phase reactants
significant increase was found of interlukin-1 (IL-1), interlukin-6(IL-6) and
tumor necrosis factor-a (TNF-a).
The levels of IL-1 in the subject group is significantly higher 6.19 ± 1.22 pg/ml than that of the control which is 3.45 ± 0.945 pg/ml ‘P’ value 0.015. Similarly, the IL-6 and TNF-α concentration was also found significantly high in the subjects as compared to the control group which was 10.26 ± 2.19 pg/ml and
35.26 ± 4.55 pg/ml respectively while in control subjects it was 4.22 ± 0.561 pg/ml and 21.29 ± 3.16 pg/ml respectively with p = 0.021. The mean concentrations MMP-1 and MMP-9 in their serum samples were significantly higher than the control group; MMP - 1 – 102.26 ± 7.44 ng/ml; MMP - 9- 306.25 ± 8.16 ng /
ml; (Mean
Comparisons p = 0.004 and p = 0.017).
Concentration of
Serum Lipopolysaccharide (LPS) in the subject group was higher than that of the control
group 102.25 ±
6.69 pg/ml vs 28.25 ±
3.88 pg/ml respectively, p ≤ 0.033. And finally, the level
of sRANKL was also significantly higher in subject
group (3.29 ± 0.99 ng/dl) as compare to control group (1.99 ± 0.095 ng/ dl) with p value
0.023. These findings also have implications for the role of inflammatory biomarkers genes, immune effector numbers and other matrix
disintegrating enzyme in radicular cyst biology.
4. Discussion
In
this work, there is the identification of new knowledge on the basic inflammatory and immune processes related to
radicular cysts. From the discriminant analysis of a number
of biomarkers above, it can be seen that the changes of the inflammatory
mediators, matrix metalloproteinases (MMPs) and other immune factors
in the subject groups are significantly
different from that in the control groups. These results are consistent with
the emergent knowledge of the molecular pathways that mediate cyst formation
and development in the kid kidneys. None of the systemic parameters such as
weight, age, SBP and DBP were significantly different between
control and subject groups.
This means that factors such as hypertension or obesity are not directly
correlated with the occurrence of radicular cysts in accordance to the cystic
diseases literature44.
But
the subject group showed a highly significant increase in the count of white
blood corpuscles WBC (p value = 0.011) and percentage of neutrophils (p value
0.031) suggesting an improved immunity. High WBCs and neutrophils suggest
inflammation and neutrophils are relevant in the initial
phase of defense and in the damage to cystic lesions45. The significant rise in
the level of interleukin-1 (IL-1) (p = 0.015) and interleukin-6
(IL-6) (p = 0.024) in the subject
group reaffirms the key position of these cytokines in the
inflammatory process of the radicular cysts.
IL-1 is a potent pro-inflammatory cytokine which is
We observed
the pronounced increase
of these MMPs in our study, which also corresponds to the recent investigations in which the
increased MMP activity was associated
with the aggressive behaviour of odontogenic cysts50,51. Higher
levels of LPS in the subject
group (p = 0.033) support bacterial-induced pathogenesis of radicular
cysts. LPS is a component of the outer membrane of Gram-negative bacteria,
which induce strong inflammatory response through interacting with plethora of proteins, primarily through TLR4 that results in
production of cytokines IL-1 and TNF-α52.
Studies described this bacterial component as being associated with CA strictly in terms of a source of antigens
that go on to perpetuate the immune response that enables cystic lesion growth.
LPS levels increased significantly in present study which is in consistent with
recent finding revealing the role of microbial products in the enhancement of
periapical lesions53. Soluble
receptor activator of nuclear factor kappa B ligand otherwise referred to as sRANKL,
takes part in osteoclast
differentiation and activation, which in turn results in bone resorption.
Since
we noted a highly significant increase in serum sRANKL concentration in the subject group
compared with that in the controls [mean 48.0, SD ± 2.8 vs. mean 41.8 SD ± 2.6 for the control group, p = 0.023], we conclude that the protein
is involved in the formation of RCs. SRANKL after binding with its receptor
RANK increases the activity of osteoclast precursors and stimulate bone resorption. This is evident in the process of cystic
expansion in which bone resorption enables the lesion to expand54. Recent researches presented over a decade have proved
that SRANKL is overexpressed
in periapical and radicular cysts actually demonstrating its
involvement in osteolytic processes. This can be hypothesized since
the antagonism of the SRANKL pathway may have a therapeutic
effect on the halt of cyst progression.
1.1. Pearson’s coefficient correlation matrix
The results are presented in (Table 1 and Table 2) that indicates a correlation between
clinical markers (weight,
age, systolic and diastolic blood pressure) and
biomarkers like leukocyte count, Haemoglobin, Neutrophils and other
inflammatory mediators for example IL 1,
IL, 6, TNF, α, MMP-1 and MMP-9, LPS and sRANKL. Correlation analysis
revealed that weight had a moderate relationship with systolic BP and haemoglobin; r = 0.425
and r = 0.326 respectively; thus, weight could play a role in determining BP
and Haemoglobin in patients with radicular cysts55.
These findings are in concordance with the literature
recommending the need to
control weight as a way to protect against hypertension as well as maintain
haemoglobin levels. Nonetheless, the other cytokines like IL-1, IL-6 also known to be inflammatory markers were
present in lesser intensity suggesting that weight may not play a major role
inflammatory processes occur in radicular cysts56.
Age was found however to
have a reasonably significant positive relationship with the systolic blood
pressure with 0.325 coefficient and diastolic blood pressure with a coefficient
of 0.265. This implies that there is a rise in the blood pressure with age in the patients,
these finding are in line with previous findings where age has been
identified as a strong predictor for hypertension57.
However, the present analysis
revealed that age had displayed only low significance with inflammatory
mediators such as IL-6, TNF-α etc.; it implies that, cytokine production may
not necessarily be determined by age in a situation of radicular cysts. There was a high positive correlation between cytokines; IL-1, IL-6
and TNF-α respectively, IL-6 and TNF-α had very high correlation (r = 0.958 p
< 0.001)58.
Table 1: Expression of Different Variables And Their Impending Role To Develop Radicular Cyst.
|
VARIABLES |
CONTROL (n=50) |
SUBJECTS (n=50) |
P-VALUE (<0.05) |
|
WEIGHT (Kg) |
71.59 ± 3.27 |
73.55 ± 7.55 |
0.659 |
|
AGE (Years) |
47.88 ± 3.55 |
48.07 ± 3.77 |
0.426 |
|
SBP (mmHg) |
121.19 ± 7.99 |
125.46 ± 5.48 |
0.124 |
|
DBP (mmHg) |
76.99 ± 5.56 |
76.44 ± 4.53 |
0.216 |
|
WBC (k/mcl) |
4.18 ± 0.912 |
5.44 ± 1.11 |
0.011 |
|
Hb (g/dl) |
14.05 ± 2.33 |
13.19 ± 3.16 |
0.256 |
|
NEUTROPHILS
(%) |
71.59 ± 4.29 |
109.88 ± 6.88 |
0.031 |
|
IL-1 (pg/ml) |
3.45 ± 0.945 |
6.19 ± 1.22 |
0.015 |
|
IL-6 (pg/ml) 4.22 ± 0.561 10.26 ± 2.19 |
0.024 |
||
|
TNF-α (pg/ml) |
21.29 ± 3.16 |
35.26 ± 4.55 |
0.031 |
|
MPP-1 (ng/ml) |
33.26 ± 4.28 |
102.26 ± 7.44 |
0.004 |
|
MPP-9 (ng/ml) |
40.26 ± 5.29 |
306.25 ± 8.16 |
0.017 |
|
LPS (pg/ml) |
28.25 ± 3.88 |
102.25 ± 6.69 |
0.033 |
|
sRANKL (ng/dl) |
1.99 ± 0.095 |
3.29 ± 0.99 |
0.023 |
Table 2: Pearson S’ Correlation Coefficients Matrix Of Different Variables And Their
Impending Role To Develop Radicular Cyst.
|
VARIABLES |
weight |
age |
SBP |
DBP |
WBC |
Hb |
Neut. |
IL-1 |
IL-6 |
TNF-α |
MPP-1 |
MPP-9 |
LPS |
sRANKL |
|
Weight |
|
.235 |
.265 |
.425 |
.125 |
.326 |
.125 |
.265 |
.147 |
.235 |
.126 |
.234 |
.025 |
.032 |
|
Age |
|
|
.265 |
.325 |
.235 |
.245 |
.152 |
.015 |
.023 |
.014 |
.023 |
.025 |
.321 |
.159 |
|
SBP |
|
|
|
.625** |
.184 |
.025 |
.265 |
.352 |
.014 |
.265 |
.0325 |
.014 |
.325 |
.235 |
|
DBP |
|
|
|
|
.235 |
.236 |
.235 |
.235 |
.025 |
.326 |
.014 |
.235 |
.026 |
.023 |
|
WBC |
|
|
|
|
|
.025 |
.526* |
.011 |
.235 |
.634** |
.256 |
.234 |
.214 |
.026 |
|
Hb |
|
|
|
|
|
|
.025 |
.421* |
.023 |
.525* |
.235 |
.659* |
.125 |
.652 |
|
Neutrophils |
|
|
|
|
|
|
|
.235 |
.452 |
.265 |
.211 |
.235 |
.452 |
.235 |
|
IL-1 |
|
|
|
|
|
|
|
|
.635* |
.435** |
.736* |
.835* |
.635* |
.841** |
|
IL-6 |
|
|
|
|
|
|
|
|
|
.458* |
.769** |
.958*** |
.654* |
.569** |
|
TNF-α |
|
|
|
|
|
|
|
|
|
|
.652* |
.958** |
.568* |
.565* |
|
MPP-1 |
|
|
|
|
|
|
|
|
|
|
|
.546** |
.925* |
.765** |
|
MPP-9 |
|
|
|
|
|
|
|
|
|
|
|
|
.658* |
.661** |
|
LPS |
|
|
|
|
|
|
|
|
|
|
|
|
|
.856* |
|
sRANKL |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
These
relationships suggest that inflammatory processes in the development of radicular
cysts are very interdependent. IL-6 also showed significant correlation
with the MMPs which are MPP-1, r = 0.769, p < 0.01 and with MPP-9, r = 0.958,
p < 0.001;
these proteins play a major role of matrix turnover which is a key factor in cyst growth and tissue degeneration59. We observed a significant positive correlation with matrix metalloproteinases particularly MPP-9 with various inflammatory cytokines and LPS which were IL-6 (r = 0.958; p < 0.001) and TNF- α (r = 0.568;p < 0.01). Moreover, MPP-9’s positive association with sRANKL (r = 0.856; p < 0.01) support the observation that this protein is involved in bone resorption and tissue repair, essential in the formation of radicular cysts60. Lipopolysaccharide (LPS), a bacterial endotoxin, revealed a statistically significant positive correlation with sRANKL (r = 0.856; p < 0.01); thus, bacterial infection may be involved in the activation indifferent RANKL signalling pathway in the bone resorption shown in radicular cysts. Moreover, a moderate relationship between sRANKL and other inflammation mediators including IL-1 (r = 0.841, p< 0.01) and IL-6 (r = 0.569, p < 0.01) also supports the notion that inflammation and remodelling are cardinal cystogenic events. The following clinical research variables have presented material facts, as illustrated in this correlation matrix analysis these findings attempt at establishing new-a-pert relationship between clinical variables, inflammatory markers and matrix metalloproteinases concerning the pathophysiology of radicular cysts. Such insights may help design new therapy approaches that may engage anti-inflammatory and tissue remodelling signals in order to improve the management and treatment of radicular cysts.
5. Conclusion
Altogether, it is clear from his present work that there is an intricate kinetic relationship between the inflammatory mediators among the individual bacterial components within the cysts as well as the matrix-degrading enzymes. The increased concentration of IL-1, IL-6, TNF-α, MMP-1, MMP-9, LPS and sRANKL indicate that inflammation, tissue degradation and bone resorption are the main processes that contribute to the growth of cystic lesion. These results are in consonance with recent developments in the knowledge of periapical diseases and may hold salutary therapeutic implications for the cure of radicular cysts. The current study projects the role of LPS in the activation of inflammatory cytokines and MMPs. The raised levels of LPS in patient group might increase the levels of MMPs and cytokines resulting in the degradation of bone matrix and basement membrane which may contribute in the development of radicular cyst. The results of present study may conclude that higher levels of MMP-1 and MMP-9 are actively involved in the destruction of periapical tissue and pathogenesis of radicular cyst. This study opens a new window of opportunity for the diagnosis, monitoring and treatment of chronic periapical lesions. Further studies are required to establish the destructive role of MMPs in periapical lesions while inhibitors of matrix metalloproteinases may be of clinical use in the treatment of radicular cyst.
5.1.1. Ethics approval and consent to participate: All the
participants were informed of the purpose of the study, methods to be used,
possible harms and benefits, besides any adverse effects of participating in
the study were explained to the participants and the participants made their
contribution willingly. All participants’ identities were kept confidential and their privacy was respected;
information gathered was also aggregated in order to maintain anonymity.Bottom
of Form
5.1.2. Consent of publication
We
confirm that this work represents original research and has not been published
previously and is not under submission for publication elsewhere. Further, all
the participants have given their informed consent for using anonymous data in
publications that will emanate from this research. All names, places
organizations and other details have been disguised to provide the users’
anonymity and institutions’ anonymity. The authors also understand and adhere to the Publication Statement of the journal and make a voluntary consent to undergo
the editorial process involved in the reviewing and publishing of this piece of
work.
5.1.3. Availability of data and materials
The
datasets generated and/or analysed during the current study, titled “Unveiling
the Enigmas of Radicular Cysts: The raw data or raw facts and the PowerPoint
presentations, which were slides; “Perception of Their Development Journey: A New Perspective on Their Development and Progression”, can be
For
further inquiries or access to the datasets and materials, please contact:
Prof. Dr. Arif Malik
Email: [email protected]
Cell:0321-8448196
6. Conflict of interest
Authors declare
no conflict of interest.
7. Funding
This
research work, is supported by Department of ORIC, The University of Lahore,
Lahore-Pakistan under grant (1970:/ SPRM/UOL/2345). The specific funding source
had no part in the study design,
data collection, analysis
of data, interpretation of data or in the
preparation of this manuscript.
8. Author’s contributions
Conception
and design of the study: AM and MW. Acquisition of data, analysis and
interpretation of data: JI, AZ and MW. Drafting the article: AM, JI, MW, AZ.
Revising the article critically for important intellectual content: AM, JI, MW,
AZ. Final approval of the version to be submitted: AM and MW. All
authors contributed equally
and have read and agreed
to the published version of
the manuscript.
9. Acknowledgement
The authors
are highly thankful
for the valuable contribution
of students of LAB-313, School of Pain and regenerative Medicines (SPRM), The
University of Lahore-Pakistan for the completion of the manuscript.
10. References
1. Nair PNR. Non-microbial etiology: Periapical cysts sustain post treatment apical periodontitis. Endodontic Topics,
2003;6:96- 113.
2. Singh HP, Shetty DC, Wadhwan V, Aggarwal P. A quantitative and qualitative comparative analysis of collagen
fibers to determine the role of connective tissue stroma on
biological behaviour of odontogenic cysts: a histochemical
study. Natl J Maxillofac Surg, 2012;3:15-20.
3. Manne R, et al.
“Histopathological correlation of inflammatory markers in radicular cysts.”
Journal of Investigative and Clinical
Dentistry, 2018.
4. León B, et al. MMP-9 levels
in periapical lesions:
An indication of inflammation and tissue destruction. Clinical Oral Investigations, 2019;23:2655-2662.
5. Samanna V, Ma T, Mak TW, Rogers M, Chellaiah MA.
Actin polymerization modulates CD44 surface expression, MMP-9 activation and osteoclast function. J Cell Physiol, 2007;213:710- 720
6. Narula H, Ahuja B, Yeluri R, Baliga S, Munshi
AK. Conservative non-surgical management of an infected radicular cyst. Contemp Clin Dent, 2011;2:368-371.
7. Latoo S, Shah AA,
Jan SM, Qadir S, Ahmed I, PurraAR,
Malik AH. Radicular Cyst. JK Science, 2009;11:187-189.