A Closed-Loop Audit of Thrombo-Embolic Deterrent Stocking Use in an Orthopaedic Ward
Abstract
Background/Objective: In Ireland, 63% of venous thromboembolism (VTE) cases develop in hospitals. In orthopaedics, 45 – 51% of inpatients develop deep vein thrombosis without adequate thromboprophylaxis. Thrombo-embolic deterrent stockings (TEDS) exert circumferential pressure, reducing venous diameter, increasing venous blood flow and limiting venous distension. Correct use maximises benefits while incorrect use can cause constriction and distal stagnation
This audit aimed to assess patient adherence to the correct use of Thrombo-Embolic Deterrent Stocking (TEDS) and whether they had received the appropriate education regarding TEDS
Methods: This closed-loop audit was conducted in the orthopaedic ward of a teaching hospital in Dublin, Ireland. Phase one was conducted over two weeks in June 2023 and phase two was conducted over two weeks in September 2023. Each phase involved collecting data from 20 patients. An educational intervention was conducted between each phase to remind ward staff to monitor patient adherence to TEDS and educate patients regarding the importance of TEDS. An educational poster was also created.
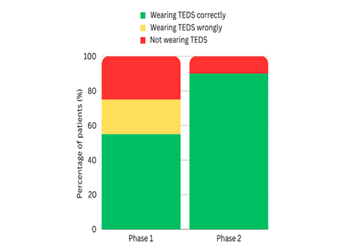
Results: Phase one revealed that only 55% of patients were wearing TEDS correctly and only 65% were educated on the importance of TEDS. In phase two, after the educational intervention, there was an improvement in patient adherence and knowledge. 90% were wearing TEDS correctly and 80% had been properly educated.
Conclusion: This audit showed that monitoring and education are vital in improving patient adherence to wearing TEDS. Evidence shows that mechanical thromboprophylaxis is beneficial in reducing thromboembolic events. Regular audits should be continued to ensure these behaviors are maintained.
Keywords: Anti‐embolism stockings; Deep vein thrombosis; Surgical patient; Thromboembolism deterrent; Venous thromboembolism
The pathophysiology of VTE is attributed to Virchow’s triad: intravascular vessel wall damage, stasis of blood flow and hypercoagulability4-6. Given that the causes and risk factors of VTE are well documented, 70% of healthcare-related VTE can be prevented by appropriate VTE prophylaxis2. Pharmacological prophylaxis involves using drugs such as low molecular weight heparin while mechanical prophylaxis involves thrombo-embolic deterrent stockings (TEDS) or intermittent pneumatic compression pumps7. Even without immobilization, hospitalized patients have greatly reduced physical activity and increased sedentary behavior which increases stasis8-10. A study by Meester’s et al. (2018) of 336 patients aged 18 years or older who were hospitalized for more than 3 days found that patients were physically active on less than 35% of their time spent hospitalized, showing that both older adult and adult patients are physically inactive during their hospitalisation9. According to a systematic review by Kirk et al. (2020), patients engaged in 1.3 to 5.9 times more physical activity and 67% less daily sedentary after discharge from to while they were in the hospital10. TEDS overcome stasis by exerting circumferential pressure on the calf, reducing the diameter of veins and, by Poiseuille’s law, increasing venous blood flow11. This pressure also limits venous distension, preventing micro-endothelial trauma11. TEDS must be used properly to maximize benefits and become problematic when used incorrectly because rolled or bunched stockings cause constriction and distal stagnation12.
This audit aims to assess whether orthopedic surgery inpatients are effectively using TEDS and whether they have received the appropriate education regarding TEDS. It also aims to serve as a pilot study of the effectiveness of the educational intervention in improving ward-based practices and set a precedent for future audits.
Methods
Setting
An
audit of orthopedic inpatients in an orthopedic specialty ward of St. James’s
Hospital, a teaching hospital in Dublin, was conducted on two occasions. Verbal
consent from patients was obtained for this audit. This audit was approved by
the Tallaght University Hospital and St James’s Hospital Research Ethics
Committee. The ward has around 15 – 20 orthopedic patients at any point in
time. Therefore, a sample size of 20 was chosen to provide a snapshot of the
ward at a random point in time. Patients were only visited once. Patients in
which TEDS were contraindicated and patients who were unavailable at the time
of the audit, severely unwell, cognitively impaired or unable to communicate
were excluded. An audit tool was created with the advice of the senior author (Table
1).
Table
1:
TEDS Audit Tool
|
Date: |
Patient Number: |
|
Gender: M / F |
Age: |
|
Reason for admission: |
|
|
Number of post-operative days: |
|
|
Mobilisation status: immobile / limited mobility /
independently mobile |
|
|
Pharmacological thromboprophylaxis: |
|
|
Is the patient wearing TEDS? If not, why? |
|
|
Does the patient have correctly sized TEDS? |
|
|
Was the patient told why they need TEDS? |
|
|
Abbreviations: TEDS = thrombo-embolic deterrent
stockings |
|
Standards
The audit standard selected
was the Health Service Executive’s (HSE) “Preventing Blood Clots in Hospitals”
guidelines and the National Institute for Health and Care Excellence's (NICE)
“venous thromboembolism in over 16s: reducing the risk of hospital-acquired
deep vein thrombosis or pulmonary embolism” guidelines. Both state that all
surgical patients must use correctly fitted TEDS unless contraindicated and
patients must receive verbal information on thromboprophylaxis while NICE
guidelines further indicate that patients should wear TEDS Day and night until
mobility is restored and that the proper wearing of stockings and assistance in
rectifying problems should be conducted2,7.
Contraindications include congestive heart failure, peripheral arterial
disease, severe dermatitis, massive leg oedema, leg deformities, peripheral
neuropathy, recent skin graft, fabric allergy or acute stroke2,7. The following standards were set: 1) 100%
of surgical inpatients should always be wearing TEDS unless contraindicated; 2)
100% of patients should be wearing correctly sized TEDS; and 3) 100% of
patients or families should be educated on why they need to wear TEDS.
Data Collection
Phase one was initiated in
June 2023 and conducted over two weeks. Data collected included gender, age,
reason for hospitalisation, days post-surgery, pharmacological
thromboprophylaxis and mobilisation status categorised into the following
subgroups: immobile being bed or wheelchair-bound, limited mobility requiring
walking aids or nursing assistance and independently mobile. Adherence to TEDS
was assessed by checking whether patients were wearing them at the time. Legs
were measured with single-use measuring tapes and stockings were checked to be
correctly sized and worn properly. The stockings were checked to be fit well on
patient’s legs to ensure they were not too loose or too tight. Limbs were
measured according to manufacturer guidelines: calf circumference at the
greatest point and the length from the back of the heel to the bend in the knee
were measured. Incorrect use of stockings was corrected. Examples of incorrect
use include bunching, rolling, folding and repression of toes. Patients who were
not wearing stockings were asked for the reasons why and were encouraged to
wear them. Sizes of unworn stockings kept at the bedside were also checked.
Patients were asked if they were educated on why TEDS were necessary.
Intervention
After phase one, an
educational intervention was undertaken. Results were discussed with the
clinical nurse manager. Nurses were reminded to monitor patient adherence and
to replace soiled or damaged stockings. An educational poster was created and
strategically placed at the nursing station (Figure 1). Phase two was
initiated in September 2023 and conducted over two weeks.
Figure 1: Educational Poster
Statistical Analysis
A
Chi-Square (X2) test was used to analyse nominal data. P-values lower than 0.05
were considered significant. Chi-Square results were reported as: X2 (degrees
of freedom, N = sample size) = Chi-Square statistic value, p = p-value.
Statistical analysis was performed using the Statistical Software for Social
Sciences (SPSS) version 28 (IBM Inc., Armonk, New York).
Results
Demographics
In
phase one, 20 patients were audited, 11 females and nine males. The mean age
was 59.4 years (range 23 – 89 years). 17 patients were admitted for lower limb
conditions, 12 being fracture-related. Five patients were immobilised, 13 had
limited mobility and two were independently mobile. 19 patients were
post-surgery, ranging from 1 to 60 days post-surgery. One patient was
pre-surgery. 16 patients were receiving subcutaneous Heparin injections and one
was receiving oral anticoagulants. One patient awaiting surgery that day and
two patients who had just returned from surgery were not receiving
pharmacological thromboprophylaxis.
In
phase two, 20 patients were audited, 14 females and six males. The mean age was
75.2 years (range 23 – 91 years). 19 patients were admitted for lower limb
procedures, 16 being fracture-related. Seven patients were immobilised, 12 had
limited mobility and one was independently mobile. 18 patients were
post-surgery, ranging from 1 to 28 days post-surgery. Two patients had been
admitted for non-operative management. 16 patients were receiving subcutaneous
Heparin injections and four were receiving oral anticoagulants. These patient
demographics are summarised in (Table 2).
Table 2: Patient Demographics
|
|
Phase 1 |
Phase 2 |
|
Gender (males: females) |
9 : 11 |
6 : 14 |
|
Age (mean years ± SD) |
59.4 ± 18.7 |
75.2 ± 15.5 |
|
Post-operative days (mean days ± SD) |
8.53 ± 14.3 |
8 ± 7.1 |
|
Lower limb related admissions (n) |
17 |
19 |
|
Lower limb fractures (n) |
12 |
16 |
|
Upper limb related admissions (n) |
3 |
1 |
|
Upper limb fractures (n) |
3 |
1 |
|
Immobile (n) |
5 |
7 |
|
Patients with limited mobility (n) |
13 |
12 |
|
Independently mobile patients (n) |
2 |
1 |
|
Post-operative patients (n) |
19 |
18 |
|
Patients receiving subcutaneous heparin injections
(n) |
16 |
16 |
|
Patients receiving oral anticoagulants (n) |
1 |
4 |
|
Abbreviations: SD = standard deviation |
||
Patient Adherence
In
phase one, five (25%) patients were not wearing stockings and four (20%) were
wearing stockings incorrectly. Among patients not wearing stockings, two
complained that their stockings were uncomfortable or painful to wear, one had
lost their stockings and two did not think they were important. Among patients
wearing stockings incorrectly, three displayed bunching of the upper band and
one had the upper band below their mid-calf level. Patients who were wearing
stockings or had them at their bedside had all been issued correctly sized
knee-length stockings.
Phase two yielded a significant improvement in patient adherence. 2 (10%) patients were not wearing stockings. One patient said that the TEDS were uncomfortable and that he had taken them off two days before while the other claimed to have not received any TEDS since her admission. Among the 18 patients who were wearing TEDS, all had been issued correctly sized stockings. These results are illustrated in (Figure 2).
Figure 2: Stacked column comparing patient adherence in phases 1 and 2 of the audit
Patient Education
In
phase one, seven (35%) patients were not informed why they needed to wear TEDS.
There was also a slight improvement in patient education in phase two where
only 4 (20%) patients were uninformed. These results are illustrated in Figure
3.
Figure 3: Stacked column comparing patient knowledge in phases 1 and 2 of the
audits
Statistical Analysis
Regarding
adherence, in phase one, 11 (55%) patients were wearing TEDS correctly while in
phase two, 18 (90%) were wearing TEDS correctly. There was a significant
difference between phase one and two for patient adherence to wearing TEDS
correctly (55% vs. 90%; X2 (1, N = 40) = 6.14, p = 0.01).
Regarding knowledge, in phase one, 13 (65%) of patients knew why they were prescribed TEDS while in phase two, 16 (80%) knew why they were prescribed TEDS. There was no significant difference between phase one and two for patient knowledge regarding why they were prescribed TEDS (65% vs. 80%; X2 (1, N = 40) = 1.13, p = 0.3).
Other Findings
Discussing
the results of this audit with the nurses revealed that they lacked the means
to record the monitoring of patient adherence to the use of TEDS or whether
patients were educated, explaining the lack of accountability. Electronic
records of mechanical thromboprophylaxis only logged skin or stocking changes.
Patients also did not receive any written information on TEDS and were not
taught how to wear them independently, relying on nurses even if they had full
upper limb function. Nurses stated that there are no hospital guidelines
regarding teaching patients how to use TEDS or issuing educational patient
information leaflets (PILs)
DISCUSSION
Phase one of this audit revealed gaps in
management concerning adherence and knowledge. Phase two demonstrated that
monitoring and education by ward staff are vital in improving patient adherence
to wearing stockings. Studies agree that education is central to increasing
patient compliance with TEDS, in and out of the hospital13-15. Ward staff have to be responsible for ensuring necessary steps are
taken to ensure patient adherence to TEDS so that patients can receive optimal
treatment outcomes14.
VTE is the most common preventable cause of postoperative death16. Death due to PE occurs within a few hours after the onset of symptoms with a mortality rate of 15.2% if the patient presents with arterial hypotension, 24.5% if the patient is in cardiogenic shock and 90% in cardiac arrest-related PE, even with thrombolysis17. According to a systematic review by Kakkos et al. (2022), combining mechanical and pharmacological thromboprophylaxis modalities had a lower incidence of DVT than mechanical thromboprophylaxis methods alone (2.03% versus 3.81%; p = 0.0001)16. Combining mechanical and pharmacological thromboprophylaxis modalities also had a lower incidence of PE than mechanical thromboprophylaxis methods alone (0.65% versus 1.34%; p = 0.02) [16]. A systematic review by Sachdeva et al., (2018) found that compression stockings reduce the risk of DVT in general and orthopedic surgery patients, regardless of background thromboprophylaxis18. There was a 1% incidence of proximal DVT in patients using graduated compression stockings (GCS) compared to a 5% incidence among patients in a control group without GCS (p < 0.001)18. There was a 2% incidence of PE in patients using GCS compared to a 5% incidence among patients in a control group without GCS (p = 0.04)18. A systematic review by Sobieraj et al., (2013) also found that mechanical thromboprophylaxis reduces the risk of DVT when used with pharmacological thromboprophylaxis compared to pharmacological methods alone19. Autar (2009) concluded that TEDS reduce post-operative DVT by 57 – 64% when used alone and by 80% when used as an adjuvant20. A study of patients undergoing primary hip and knee arthroplasties by Gill et al., (2020) found that VTE rates in early mobilization and mechanical thromboprophylaxis were comparable to rates in pharmacological thromboprophylaxis21. A study of elective hip surgery patients by Sugano et al., (2009) found that the incidence of fatal or symptomatic PE was much lower in patients receiving mechanical thromboprophylaxis compared to similar patient populations in the literature that did not receive thromboprophylaxis, allowing them to conclude that mechanical thromboprophylaxis even without concurrent pharmacological thromboprophylaxis was safe and effective22. Furthermore, a benefit of mechanical thromboprophylaxis methods is that they do not have the same bleeding-related side effects as pharmacological methods16. Compression stockings reduce the risk of thrombosis by increasing the velocity and volume of blood flow in deep veins via circumferential pressure which displaces blood from superficial to deep circulation via perforators18. This mechanical reduction of venous stasis is thus expected to reduce the risk of VTE when combined with pharmacological anticoagulants16. However, the graduated compression as an adjunct to thromboprophylaxis in surgery (GAPS) trial by Shalhoub et al. (2020) which included 1,858 patients in an intention-to-treat analysis found that VTE up to 90 days after surgery occurred in 1.7% of patients who received pharmacological thromboprophylaxis alone in the form of low-molecular-weight heparin compared to 1.4% of patients who received both pharmacological and mechanical thromboprophylaxis in the form of GCS (p < 0.001), indicating that pharmacological thromboprophylaxis alone is non-inferior to a combination of pharmacological and mechanical thromboprophylaxis and concluding that GCS may be unnecessary for most elective surgical patients23. Autar (2009) thus emphasized that given the divided opinion of clinicians on the efficacy of TEDS despite supportive evidence, there is a great need for clinicians to continue auditing the efficacy of such mechanical thromboprophylaxis methods20.
This audit found that the educational intervention reminding ward staff to check that patients were adhering to TEDS and educating patients was effective in improving patient adherence and understanding of the importance of TEDS. Ward-based educational interventions targeted at staff are an effective means of steering change in staff behaviors and practices24-26. Oberai et al. (2021) found that an educational program for nurses on delirium prevention and management yielded improvements in knowledge of the risk factors of delirium and how to recognize delirium24. Wand et al. (2014) found that lectures and weekly interactive tutorials for medical and nursing staff with delirium resource staff and ward modifications yielded improvements in objective knowledge of delirium and confidence in assessing and managing delirious patients25. Tabet et al. (2005) found that a ward that received an educational package for medical and nursing staff which included formal presentations, group discussions, written management guidelines and follow-up one-to-one or group discussions recognized significantly more delirium cases and had a significantly reduced point prevalence of delirium compared to a control ward that did not receive the same educational package (9.8% versus 19.5%; p < 0.05)26. In addition to its primary goals, this audit also found that current hospital-wide electronic documentation of mechanical thromboprophylaxis was lacking compared to the documentation of pharmacological methods. As such, a simple yet effective documentation system could be adopted to enable consistent assessment and accountability, noting vital guiding factors such as limb measurements, sizes of stockings and any contraindications or adverse events14.
NICE guidelines further indicate that patients should be taught how to wear their stockings if possible and receive written information7. PILs have been found to improve patient adherence and knowledge in varying treatment and clinical situations27-29. Structured verbal advice along with PILs also has a significant effect on patient awareness and knowledge30. A study of 1,138 adult patients by Al Jeraisy et al. (2023) reported that 70.6% of participants said that PILs add to their knowledge of medicines and 64.9% of participants said that PILs positively impacted their medication adherence28. Sustersic et al. (2019) found that among 324 patients, those who received a PIL about their condition along with an oral explanation had a higher mean doctor-patient communication score compared to those who did not receive PILs (p < 0.01) while satisfaction with healthcare professionals and timing of medication intake improved with PILs29. In addition to PILs, educational interventions that target patients have also proven effective in other studies31. For example, see et al. (2014) found that a brief education session improved patient self-efficacy in recognizing and reporting acute symptoms of deterioration31. We thus recommend that concise and informative PILs regarding TEDS be created and distributed to patients to reinforce the need to continue wearing TEDS. According to Lim and Davies (2014), the 30 - 65% non-compliance rate for GCS can be attributed to pain, discomfort, difficulty wearing stockings, perceived ineffectiveness, heat, skin irritation and cosmetic appearance32. They further suggest that patients be informed why they were prescribed stockings, the benefits of wearing them, how to wear them correctly, how long to wear them for and when to replace them, how to maintain proper hygiene, how to recognize potential problems with stockings and who to contact should any problems be identified32. Therefore, although it is difficult to monitor patient adherence post-discharge and hospital guidelines only state the need for TEDS up to the time of discharge, PILs could potentially encourage patients to continue using TEDS while at home, especially since VTE risk continues up to 6 weeks post-discharge33.
Future directions
This closed-loop audit showed that the
ward-based educational intervention was successful in improving both patient
adherence to TEDS and understanding of their importance. For an intervention
that relies as heavily on patient cooperation as TEDS, ensuring patient
compliance and understanding is paramount. Given the positive results of this
audit, we aim to introduce the intervention in other wards and repeat the audit
on a larger scale. We also aim to design and distribute PILs to patients
alongside their TEDS.
Limitations
Limitations of this audit are the sample size
and time constraints. The audit was also subject to the natural turnover of
patients in the ward. Data collection periods for both the initial audit and
re-audit were short durations of two weeks. Despite these, the results provided
a snapshot representation of typical patient behaviors on a single orthopedic
ward. Future audits aim to include other surgical wards to obtain a larger
sample size.
Declarations
Funding:
Not applicable.
Conflicts
of interest/Competing interests: Not applicable.
Ethics
approval: Our institution does not require ethical approval for
quality improvement projects.
Consent
to participate: NA
Consent
for publication: NA
Availability
of data and material: Available upon reasonable request.
Code
availability (software application or custom code):
Not applicable.
Authors'
contributions: Both authors contributed to conception
and design, acquisition, analysis and interpretation of data. BL wrote the
initial draft. Revisions were made by both authors and the final version was
reviewed by both authors.
References
1. Moheimani
F, Jackson DE. Venous Thromboembolism: Classification, Risk Factors, Diagnosis
and Management. ISRN Hematol 2011;2011:1-7.
2. Health
Service Executive: Preventing Blood Clots in Hospitals Improvement
Collaborative Report National Recommendations and Improvement Toolkit 2018.
3. Wade
R, Paton F, Rice S, et al. Thigh length versus knee length antiembolism
stockings for the prevention of deep vein thrombosis in postoperative surgical
patients; a systematic review and network meta-analysis. BMJ Open
2016;6:009456.
4. Chung
I, Lip GYH. Virchow’s Triad Revisited: Blood Constituents. Pathophysiol Haemost
Thromb 2003;33:449-454.
5.Bagot
CN, Arya R. Virchow and his triad: a question of attribution. Br J Haematol
2008;143:180-190.
6. Kumar
DR, Hanlin E, Glurich I, Mazza JJ, Yale SH. Virchow’s Contribution to the
Understanding of Thrombosis and Cellular Biology. Clin Med Res 2010;8:168-172.
7. The
National Institute for Health and Care Excellence. Recommendations | Venous
thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein
thrombosis or pulmonary embolism - Guidance - NICE 2019.
8. Jawad
BN, Petersen J andersen O, Pedersen MM. Variations in physical activity and
sedentary behavior during and after hospitalization in acutely admitted older
medical patients: a longitudinal study. BMC Geriatr 2022;22:1-10.
9. Meesters
J, Conijn D, Vermeulen HM, Vliet Vlieland TPM. Physical activity during
hospitalization: Activities and preferences of adults versus older adults
2018;35:975-985.
10. Kirk
AG, Behm KJ, Kimmel LA, Ekegren CL. Levels of Physical Activity and Sedentary
Behavior During and After Hospitalization: A Systematic Review. Arch Phys Med
Rehabil 2021;102:1368-1378.
11. Weinberger
J, Cipolle M. Mechanical Prophylaxis for Post-Traumatic VTE: Stockings and
Pumps. Curr Trauma Rep 2016;2:35-41.
12. Miller
JA. Use and wear of anti‐embolism stockings: a clinical audit of surgical patients. Int Wound J
2011;8:74.
13. Walker
L, Lamont S. The use of ant embolic stockings. Part 1: a literature review.
British Nursing 2007;16:1408-1412.
14. Miller
JA. Use and wear of anti-embolism stockings: a clinical audit of surgical
patients. Int Wound J 2011;8:74-83
15. Donnelly
T, McNeely B. The Shocking Stocking Audit: An Audit on the Use of
Thromboembolic Deterrent Stockings (Teds) for Patients Having Surgery at Sligo
Regional Hospital. J Perioper Pract 2015;25:83-86.
16. Kakkos
S, Kirkilesis G, Caprini JA, Geroulakos G, Nicolaides A, Stansby G, Reddy DJ:
Combined intermittent pneumatic leg compression and pharmacological prophylaxis
for prevention of venous thromboembolism. Cochrane Database of Systematic
Reviews 2022.
17. Hajouli
S. Massive Fatal Pulmonary Embolism While on Therapeutic Heparin Drip. J
Investig Med High Impact Case Rep 2020;8.
18. Sachdeva
A, Dalton M, Lees T. Graduated compression stockings for prevention of deep
vein thrombosis. Cochrane Database of Systematic Reviews 2018;2019:10.
19. Sobieraj
DM, Coleman CI, Tongbram V, et al. Comparative Effectiveness of Combined
Pharmacologic and Mechanical Thromboprophylaxis versus Either Method Alone in
Major Orthopedic Surgery: A Systematic Review and Meta-analysis.
Pharmacotherapy: J Human Pharma and Drug Therapy 2013;33:275-283.
20. Autar
R. A review of the evidence for the efficacy of Anti-Embolism Stockings (AES)
in Venous Thromboembolism (VTE) prevention. J Orthopedic Nursing 2009;13:41-49.
21. Gill
SK, Pearce AR, Everington T, Rossiter ND. Mechanical prophylaxis, early
mobilization and risk stratification: as effective as drugs for low-risk
patients undergoing primary joint replacement. Results in 13,384 patients. The
Surgeon 2020;18:219-25.
22. Sugano
N, Miki H, Nakamura N, Aihara M, Yamamoto K, Ohzono K. Clinical Efficacy of
Mechanical Thromboprophylaxis Without Anticoagulant Drugs for Elective Hip
Surgery in an Asian Population. J Arthroplasty 2009;24:1254-1257.
23. Shalhoub
J, Lawton R, Hudson J, et al. Compression stockings in addition to
low-molecular-weight heparin to prevent venous thromboembolism in surgical
inpatients requiring pharmacoprophylaxis: the GAPS non-inferiority RCT. Health
Technol Assess (Rockv) 2020;24:1-80.
24. Oberai
T, Laver K, Woodman R, Crotty M, Kerkhoffs G, Jaarsma R. The effect of an
educational intervention to improve orthopaedic nurses’ knowledge of delirium:
A quasi-experimental study. Int J Orthop Trauma Nurs 2021;42:100862.
25. Wand
APF, Thoo W, Sciuriaga H, Ting V, Baker J, Hunt GE. A multifaceted educational
intervention to prevent delirium in older inpatients: A before and after study.
Int J Nurs Stud 2014;51:974-982.
26. Tabet
N, Hudson S, Sweeney V, Sauer J, Bryant C, Macdonald A, Howard R. An
educational intervention can prevent delirium on acute medical wards. Age
Ageing 2005;34:152-156.
27. Sustersic
M, Gauchet A, Foote A, Bosson JL. How best to use and evaluate Patient
Information Leaflets given during a consultation: a systematic review of
literature reviews. Health Expectations 2017;20:531-542.
28. Al
Jeraisy M, Alshammari H, Albassam M, Al Aamer K, Abolfotouh MA. Utility of
patient information leaflet and perceived impact of its use on medication
adherence. BMC Public Health 2023;23:488.
29. Sustersic
M, Tissot M, Tyrant J, Gauchet A, Foote A, Vermorel C, Bosson JL. Impact of
patient information leaflets on doctor–patient communication in the context of
acute conditions: a prospective, controlled, before–after study in two French
emergency departments. BMJ Open 2019;9:024184.
30. Adepu
R, Swamy M. Development and evaluation of patient information leaflets (PIL)
usefulness. Indian J Pharm Sci 2012;74:174.
31. See
MTA, Chan W-CS, Huggan PJ, Tay YK, Liaw SY. Effectiveness of a patient
education intervention in enhancing the self-efficacy of hospitalized patients
to recognize and report acute deteriorating conditions. Patient Educ Couns
2014;97:122-127.
32. Lim
CS, Davies AH. Graduated compression stockings. Can Med Assoc J
2014;186:391-398.
33. Bratzler
DW. Development of national performance measures on the prevention and
treatment of venous thromboembolism. J Thromb Thrombolysis 2010;29:148-154.