A Rare Primary Inferior Lumbar Hernia Treated by Transperitoneal Laparoscopy: Case Report and Literature Review
Abstract
Background
Lumbar hernias are rare defects of the posterior
abdominal wall, accounting for less than 2% of all abdominal hernias, with
fewer than 400 cases reported in the literature. They arise through anatomical
weak points—either the superior (Grynfelt-Lesshaft) or inferior (Petit) lumbar
triangles-and often present a surgical challenge due to the limited
availability of healthy tissue for reconstruction. Advances in minimally
invasive surgery have made laparoscopic repair, through either a
transperitoneal or extraperitoneal approach, an increasingly preferred option.
Case Presentation
We report the case of a 56-year-old man with diabetes
who presented with a painful, reducible swelling in the left lumbar region. He
had no history of trauma, prior surgery or bowel obstruction. Physical
examination revealed a soft, non-inflammatory mass. Abdominal CT scan
demonstrated a left lumbar hernia measuring 38 × 81 mm, with a 26-mm neck and
containing only fat. Given the symptomatic presentation and favorable anatomy,
a transperitoneal laparoscopic repair was performed. After mobilization of the
descending colon from the abdominal wall, the defect was identified and closed
with sutures. A 15 × 20-cm mesh was placed to reinforce the repair and secured
using 5-mm absorbable laparoscopic tacks. The postoperative course was
uneventful and the patient was discharged on postoperative day three without
complications.
Conclusion
This case illustrates the safety and effectiveness of
the transperitoneal laparoscopic approach for primary lumbar hernia repair.
Laparoscopy provides excellent anatomical visualization, allows secure mesh
placement and is associated with reduced postoperative pain, shorter hospital
stay and rapid recovery. As demonstrated in this patient, minimally invasive
repair represents a valuable option for the management of both primary and
acquired lumbar hernias.
Keywords: Lumbar hernia; Inferior lumbar triangle; Laparoscopic
repair; Transperitoneal approach; Abdominal wall hernia; Rare hernia
Introduction
Lumbar
hernias are rare defects of the posterior abdominal wall, accounting for less
than 1-2% of all abdominal wall hernias1.
The first description of a lumbar hernia was reported by Barbette in 16722. These hernias occur when intra-abdominal,
intraperitoneal or retroperitoneal contents protrude through an area of
weakness in the posterior abdominal wall.
Anatomically,
lumbar hernias are classified according to the location of the defect: superior
(Grynfeltt–Lesshaft triangle) or inferior (Petit’s triangle). They may be
congenital or acquired, the latter being more common3.
Diagnosis
is often suggested clinically but is best confirmed by computed tomography
(CT), which allows precise assessment of the defect and helps differentiate it
from other masses. Surgical repair is the treatment of choice. However, repair
can be challenging due to the limited local tissue for reinforcement and the
proximity of bony structures. Both open and laparoscopic techniques have been
described, including transabdominal and extraperitoneal approaches.
Herein,
we report a case of a spontaneous inferior lumbar hernia successfully treated
by a transperitoneal laparoscopic approach.
Case Report
A
56-year-old man with a medical history of diabetes presented with a gradually
enlarging left lumbar swelling associated with effort-related pain. He had no
gastrointestinal symptoms, no signs of bowel obstruction and no history of
trauma or prior surgery in the lumbar region.
Physical
examination revealed a soft, reducible left lumbar mass without inflammatory
signs (Figures 1 and 2).
Figures 1 and 2: a soft, reducible left lumbar mass without inflammatory signs, measured 80 mm
A
contrast-enhanced abdominal CT scan demonstrated a 38 × 81 mm left lumbar
hernia containing adipose tissue. The hernia neck measured 26 mm and no
visceral content was noted (Figures 3 and 4).
Figure
3: (Computed tomography scan coronal view) Figure 4: (Computed tomography scan
axial view)
Figures
3, 4: A contrast-enhanced abdominal CT scan demonstrated a 38 × 81 mm left
lumbar hernia containing adipose tissue. The hernia neck measured 26 mm and no
visceral content was noted
Given
the reducibility of the hernia and the patient’s symptoms, a laparoscopic
transperitoneal repair was planned. The patient was positioned in a
semi-lateral decubitus position. Three trocars were placed: subxiphoid,
periumbilical and suprapubic. The descending colon was carefully mobilized off
the lateral abdominal wall due to its proximity to the defect (Figure 5).
Figure
5: Trocars placement
The
hernia orifice was clearly identified and closed with non-absorbable sutures. A
15 × 20 cm prosthetic mesh was positioned to reinforce the defect and secured
using 5 mm absorbable laparoscopic tacks (Figures 6-10).
Figure
6: Intra operative view of the lumbar hernia. The hernia orifice was
clearly identified

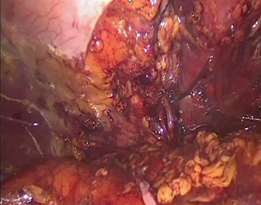
Figures
7,8: The hernia orifice was identified and closed with non-absorbable
sutures
Figure
10: A 15 × 20 cm prosthetic mesh was positioned to reinforce the defect and
secured using 5 mm absorbable laparoscopic tacks
The
postoperative course was uneventful. The patient was discharged on
postoperative day 3. At six-month follow-up, he remained asymptomatic with no
evidence of recurrence (Figure 11).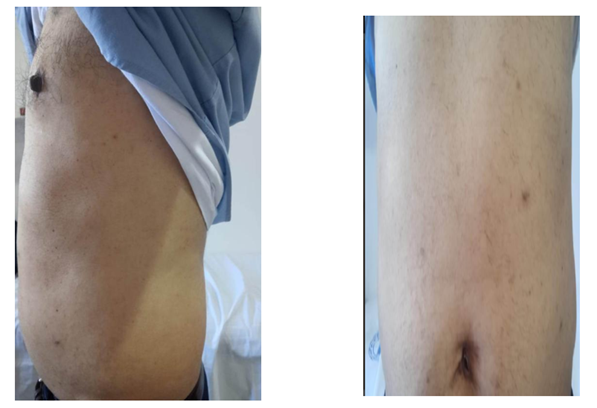
Figures
10, 11: The result after 6 months of follow-up with no recurrence
Discussion
Lumbar
hernias are an uncommon form of abdominal wall defect, representing less than
1–2% of all abdominal wall hernias4.
They tend to occur more frequently in men and are reported predominantly on the
left side, although the reasons for this lateral predominance remain unclear3. Anatomically, the posterior abdominal
wall contains two areas of natural weakness that predispose to herniation. The
superior lumbar triangle (Grynfeltt-Lesshaft triangle) is bounded superiorly by
the 12th rib, medially by the quadratus lumborum muscle and laterally by the
posterior border of the internal oblique muscle. Its floor is formed by the
transversalis fascia, while the roof consists of the external oblique muscle.
The inferior lumbar triangle (Petit’s triangle), by contrast, is defined
anteriorly by the external oblique muscle, posteriorly by the latissimus dorsi
muscle and inferiorly by the iliac crest. Weakness within either of these
anatomical triangles may allow retroperitoneal or intraperitoneal contents to
protrude, giving rise to a lumbar hernia. Understanding the structural
boundaries and intrinsic vulnerabilities of these regions is essential for
accurate diagnosis and for planning the most appropriate surgical approach.
Etiology
Lumbar hernias may be congenital, representing
about 20% of cases or acquired, accounting for nearly 80% of all presentations5. Acquired lumbar hernias are further
classified as either primary or secondary. Primary (spontaneous) hernias
develop without any preceding trauma or surgery and are often associated with
factors such as aging, chronic increases in intra-abdominal pressure, chronic
cough, heavy lifting, obesity or extreme thinness. In contrast, secondary
hernias arise as a consequence of trauma, previous surgical
procedures—particularly iliac crest bone graft harvesting-local infections or
muscle atrophy. In the present case, the patient exhibited none of the
predisposing events or surgical history typically associated with secondary
hernias, supporting the diagnosis of a primary spontaneous lumbar hernia.
Clinical presentation
Patients with lumbar hernias may present with
nonspecific or subtle symptoms, which often contribute to delayed diagnosis and
misinterpretation. The most frequent clinical finding is a soft, posterolateral
swelling in the lumbar region that may increase with coughing or straining and
may or may not be reducible. Some patients report vague, intermittent lower
back or flank pain due to traction on surrounding tissues. Although
incarceration or strangulation is considered uncommon, several authors have documented
these complications, emphasizing the importance of early detection and
appropriate management1,2.
Because their presentation may resemble more common conditions-including
lipomas, abscesses or soft-tissue tumours-lumbar hernias require a high index
of suspicion for accurate diagnosis3.
In our case, the patient presented with a well-defined swelling located in the
inferior lumbar triangle on the left side, progressively enlarging over one
year.
Diagnosis
Although
the diagnosis may be suggested clinically, CT scan remains the gold standard
imaging modality. It provides detailed information regarding the size of the
defect, content of the hernia sac and helps exclude differential diagnoses such
as lipoma, rhabdomyoma, hematoma or sarcoma6.
In
our case, the CT scan demonstrated a well-defined posterolateral defect located
in the inferior lumbar triangle on the left side, with protrusion of
preperitoneal fat into the subcutaneous tissues. The hernia sac contained no
bowel loops and there were no signs of incarceration or inflammatory changes.
The detailed CT findings confirmed the diagnosis of a primary lumbar hernia and
guided the surgical strategy by clearly illustrating the dimensions of the
defect and its relationship to adjacent muscular structures.
Management
Due to the potential risk of complications-most
notably incarceration-surgical repair is generally recommended for both primary
and secondary lumbar hernias7.
The main objective of the intervention is to restore the integrity of the
abdominal wall, reinforce the weakened anatomical zone and minimize the
likelihood of recurrence. However, repair of lumbar hernias can be technically
demanding because of several anatomical constraints. The defect lies between
rigid osseous boundaries, namely the 12th rib superiorly and the iliac crest
inferiorly, which limit surgical exposure and restrict the placement of
fixation points. Additionally, the musculature in this region is often
attenuated or anatomically deficient, reducing the quality of the available
tissue for primary closure. Achieving sufficient mesh overlap is another
critical challenge, as the confined space and proximity to neurovascular
structures require careful dissection and precise positioning8.
A variety of operative strategies have been
described, ranging from direct tissue approximation and the use of rotational
muscle flaps to the more widely adopted mesh-based tension-free repairs9-11. Both open and laparoscopic approaches
have demonstrated favourable outcomes, yet no standardized technique has been
universally endorsed, largely because of the rarity of lumbar hernias and the
consequent lack of large comparative studies7.
As a result, the choice of surgical method is often individualized, taking into
account the size and location of the defect, the condition of surrounding
tissues and the surgeon’s expertise.
In our case, the hernia was repaired using an
laparoscopic approach with placement of a prosthetic mesh, allowing for secure
reinforcement of the defect and an uneventful postoperative recovery.
Laparoscopic
repair
In
recent years, laparoscopic repair has gained significant popularity in the
management of lumbar hernias, with both the transabdominal preperitoneal (TAPP)
and totally extraperitoneal (TEP) approaches demonstrating promising outcomes12. These minimally invasive techniques
offer several advantages over traditional open repair. The laparoscopic view
provides superior visualization of the anatomical structures, particularly the
boundaries of the lumbar triangles and the extent of the muscular defect, which
facilitates precise dissection and safer manipulation of surrounding tissues.
Because laparoscopic repair requires only minimal dissection, it reduces trauma
to the abdominal wall and lowers the risk of postoperative morbidity.
Another
major benefit is the ability to achieve optimal mesh placement with generous
overlap, ensuring secure coverage of the defect and reducing the likelihood of
recurrence. The minimally invasive nature of these techniques is also
associated with less postoperative pain, a lower incidence of surgical site
infections and hematomas and reduced need for postoperative analgesia13-15. Additionally, patients typically
experience a shorter hospital stay and can resume normal activities more
quickly compared to those undergoing open surgery, making laparoscopy an
attractive option whenever feasible.
In
our patient, the transperitoneal laparoscopic approach allowed safe
mobilization of the descending colon, clear visualization of the defect and
secure mesh placement. The postoperative outcome was excellent, with no
recurrence at 6 months.
Conclusion
Lumbar hernias are rare and can be easily
overlooked due to their subtle presentation. Early surgical repair is
recommended to prevent complications such as incarceration or strangulation.
The proximity of bony landmarks and the weakness of the posterior abdominal
musculature make repair technically challenging.
Laparoscopic lumbar hernia repair is a safe and
effective approach offering superior visualization, reduced postoperative pain
and faster recovery. Although no standardized surgical technique exists due to
the rarity of this condition, laparoscopic transperitoneal repair represents a
valuable and increasingly preferred minimally invasive option.
References
3. Gaillard F, El-Feky M, Rasuli B, et al. Lumbar hernia.
Reference article Radiopaedia.
7. Sharma P. Lumbar hernia. MJAFI 2009;65:178–179
9. Geis WP, Hodakowski GT. Lumbar hernia. In: Nyhus LM,
Condon RE (ed) Hernia. Lipincott, Philadelphia 1995:412-424.
14. Sundaramurthy S, Suresh HB, Anirudh
AV, Rozario AP. St. John’s Medical College Hospital, Department of General
Surgery, Sarjapur Road, Koramangala, Bangalore, Karnataka Primary lumbar
hernia: A rarely encountered hernia Sharada 2015.