Bilateral Peripheral Retinal Vasculitis in a Young Patient: A Case Report
Abstract
Bilateral peripheral retinal vasculitis is an inflammatory condition that
affects the peripheral blood vessels of the retina in both eyes. This
inflammation can lead to severe complications, such as hemorrhages, vascular
occlusions and significant visual acuity loss. The causes are varied, including
autoimmune diseases, systemic infections and idiopathic conditions. Early
diagnosis and appropriate treatment are essential to prevent permanent vision
damage.
Keywords: Vasculitis; Bilateral; Angiography;
Neovascularization
Introduction
Objective
To present a case of bilateral peripheral retinal vasculitis in a young
patient, highlighting the diagnostic and therapeutic complexity of this
condition.
Materials and Methods
Data for this study were obtained through a review of the patient's
electronic medical records. A literature review was conducted using the PUBMED
and ScienceDirect databases.
Case Report
A 25-year-old obese woman presented with sudden visual blurring in the left
eye (LE). Corrected visual acuity was 20/20 in the right eye (RE) and 20/50 in
the LE, with a refraction of -5.00 spherical in both eyes (BE). Biomicroscopy
revealed fine keratic precipitates and +1/+4 cells in the LE, with intraocular
pressure of 12 mmHg in BE. Additionally, mild vitreous hemorrhage and superior
temporal neovascularization were observed. Angiography (Figure 4) showed
capillaritis, peripheral vascular remodeling and 360° non-perfusion in BE.
There was leakage in areas of superior temporal retinal neovascularization in
the LE. Complementary tests revealed a positive IGRA and a strongly reactive
PPD. The patient was treated with a RIPE regimen for two months, followed by RI
for four months, along with oral corticosteroids with gradual regression.
Anti-VEGF therapy was administered in the LE to control neovascularization,
resulting in visual improvement and absence of neovascularization. Retinal
photocoagulation was performed in ischemic areas of both eyes. Follow-up
angiography demonstrated persistence of peripheral vasculitis. A new clinical
evaluation was requested to discuss pharmacological immunosuppression (Figures
1-8).
Figure 1: Right eye fundus: Normal appearance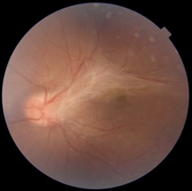
Figure 2: Left eye fundus: Epiretinal gliosis along the
superior vascular arcade, vascular tortuosity
Figure 3: Left eye fundus: Leakage in superior temporal
neovascularization
Figure 4: Angiography: Capillaritis, peripheral vascular
remodeling and 360º non-perfusion
Figure 5: Vitreoretinal interface traction, with edema and
disruption of superior retinal layers near the macula
Figure 6: Post-anti-VEGF OCT: Spontaneous improvement in
vitreoretinal interface traction, with macular structure improvement
Figures 7 and 8: Angiography: Vasculitis and increased
temporal ischemia in the right eye. Superior vasculitis areas in the left eye
Discussion
This case underscores the importance of differentiating between primary and
secondary vasculitis, emphasizing the need for a multidisciplinary approach to
diagnosis and management8-10. The persistence of vasculitis (Figure
7 and 8) after antibiotic treatment for tuberculosis suggests other
potential etiologies, such as Eales disease, autoimmune, infectious, systemic,
genetic or hematological conditions11,12. Collaboration among
specialists is essential for an accurate diagnosis and effective treatment plan13,14.
Conclusion
This case report highlights the challenges in diagnosing and treating
peripheral retinal vasculitis, emphasizing the importance of multidisciplinary
evaluation in diseases with similar findings, considering the endemic nature of
tuberculosis in Brazil.
Ethical Staatement
Informed consent has been provided by the patient for publication of this case report.
References
- Siqueira, R. C.; Oréfice,
Vasculites da Retina F. In: ORÉFICE, F. et al. Uveítes. Série Oftalmologia Brasileira. 4ed. Rio de
Janeiro: Cultura Médica, 2016;11:105-123.
- Hughes EH, Dick AD.
The pathology and pathogenesis of retinal vasculitis. Neuropathology and
Applied Neurobiology 2003;29(4):325-340.
- Ali A, Ku JH, Suler EB, et al. The
course of retinal vasculitis. British Journal of Ophthalmology
2014;98(6):785-789.
- Tahreem AM, et al.
Clinical Features and incidence rates of ocular complications in patients with
retinal vasculitis. American J Ophthalmology 2017;179:171-178.
- Rosenbaum JT,
Sibley CH, Lin P. Retinal Vasculitis. Current Opinion in Rheumatology
2016;28(3):228-235.
- Rodrigues KFP, Lima VC, Arantes TEF, Matos
KTF, Muccioli C. Retinite idiopática, vasculite, aneurismas e neurorretinite
(IRVAN): relato de caso. Arquivos Brasileiros de Oftalmologia
2012;75(2):138-141.
- Rosa A. Tudo sobre vasculite retiniana.
RetinaPro 2023.
- Lobo,
Doença de Eales RRT. Repositório
da Universidade de Lisboa 2017.
- Eoftalmo. Elaboração de protocolo de
investigação de vasculites retinianas. EOftalmo 2020;6(1):1-10.
- Gonçalves FG, Souza AS. Atualização em vasculites: visão geral e
aspectos dermatológicos. Clinics 75:2174.
- Revista Brasileira de Oftalmologia. Vasculite
retiniana. Revista Brasileira de Oftalmologia.
- Eoftalmo. Resultados da
Busca - Vasculite Retiniana. eOftalmo.
- Silva RA, Lima VC. Vasculite retiniana: diagnóstico e tratamento. Revista Brasileira de Oftalmologia 2019;78(3):183-189.
- Santos FM, Oliveira AG. Vasculite retiniana: uma revisão de literatura. J Ophthalmology 2018;12(2):45-52.