Combined Percutaneous Ethanol Injection and Radiofrequency Ablation for a Large Recurrent Cystic Thyroid Nodule
Abstract
Large predominantly cystic thyroid nodules often
respond well to percutaneous ethanol injection (PEI); however, cases with
substantial residual solid components may require adjunctive treatment. This
case study illustrates the clinical utility of combining PEI and radiofrequency
ablation (RFA) to achieve optimal therapeutic outcomes in a patient with a
symptomatic, compressive thyroid nodule not amenable to PEI alone. A
57-year-old male presented with a >180 mL predominantly cystic thyroid
nodule causing dysphagia and neck discomfort. Ultrasound-guided aspiration and
PEI were performed multiple times, however the nodule repeatedly reaccumulated
fluid. Given the suboptimal response, the patient underwent a subsequent
session of RFA targeting the solid nodule portion followed by repeat PEI. Over
a 12-month follow-up, the nodule volume decreased by >95% and the patient
experienced complete resolution of symptoms without adverse effects. This case
demonstrates that combined PEI and RFA therapy is a safe and effective strategy
for managing large predominantly cystic thyroid nodules when PEI alone is
insufficient. The synergistic use of PEI for the cystic portion followed by RFA
for residual solid tissue may offer a valuable non-surgical alternative even in
very large nodules for selected patients.
Keywords: Thyroid nodule; Percutaneous ethanol injection; Radiofrequency
ablation; Thermal ablation
Introduction
Recurrent large thyroid nodules present a
clinical challenge, particularly when conventional surgical or ablative options
are limited due to anatomical complexity or patient comorbidities. In such
cases, a combined minimally invasive approach using radiofrequency ablation
(RFA) and percutaneous ethanol injection (PEI) has shown promise. RFA offers
effective debulking of solid components, while PEI enhances treatment efficacy
by targeting residual cystic or vascular regions, reducing recurrence risk. This
case study explores the synergistic benefits of combining RFA and PEI for
managing a large, recurrent thyroid nodule that was not responsive to PEI
alone, highlighting improved volume reduction, symptom relief and procedural
safety.
Case
Presentation
56-year-old male presented to the clinic for
rapidly enlarging thyroid cystic nodule for the prior year. He was experiencing
neck discomfort especially when bending his neck forward that was worsening. He
underwent multiple aspirations of this nodule and fine needle aspiration (FNA)
biopsy performed twice was negative for malignancy. He wanted to avoid surgery
if possible.
Diagnostic assessment
Baseline evaluation and ultrasound were
performed in the office (Figure 1).

a) Photo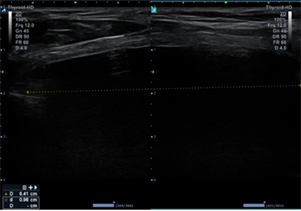
b) Ultrasound image - AP and transverse view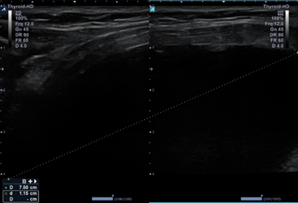
c) Ultrasound image – lateral view
Figure 1: Baseline images before
intervention
Treatment
After
initial consultation and review of all the potential treatment options, the
decision was made to aspirate the cystic nodule and perform percutaneous
ethanol injection. The cystic fluid rapidly re-accumulated. FNA and PEI were
repeated two additional times, aspirating 150 mL and 120 mL respectively. The
decision was made to repeat aspiration and perform RFA concentrating on the
complex areas adjacent to the walls of the nodule that were not easily visible
before aspiration. The amount of energy delivered was up 50 mHz with an active
ablation time of 20 minutes and 38 seconds.
Outcome
and follow-up
At one month follow-up, the patient noted
significant improvement in neck discomfort. The patient was seen in follow up
at three and six months. At twelve-month follow-up of RFA the nodule remains
stable to decreased in size to approximately 10 mL, significantly decreased in
size by more than 95% from baseline status post RFA and PEI (Figure 2). His
thyroid function tests remained normal. Discussion was made regarding repeat
intervention, but since the patient was so pleased with his status, the
decision was made to re-evaluate in one year with repeat ultrasound.
a)
Photo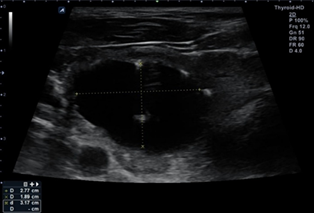
b) Ultrasound image – AP and transverse view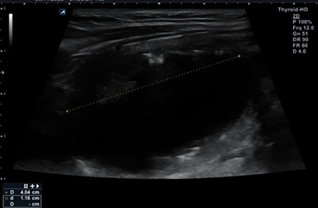
c)
Ultrasound image – lateral view
Figure 2: Images one-year post-PEI
and RFA
Discussion
Thyroid
nodules are discrete lesions within the thyroid gland that are radiologically
distinct from the surrounding parenchyma and are a common clinical finding,
with a prevalence ranging from 20% to 76% depending on the population and
detection method used1. While
most thyroid nodules are benign, approximately 5% to 15% may be malignant,
necessitating careful evaluation through physical examination, thyroid function
testing, ultrasonography and fine-needle aspiration cytology2. Risk factors for the development of
nodules include iodine deficiency, radiation exposure, advancing age and female
sex3. Most benign nodules are
non-functional and asymptomatic; however, they may cause compressive symptoms
or cosmetic concerns in some patients. Management strategies vary based on
size, growth, cytological characteristics and patient preference, ranging from
active surveillance to surgical removal. Understanding the pathophysiology and
optimal diagnostic approaches is essential for effective and individualized
treatment planning.
Treatment
options for thyroid nodules depend on the nodule’s size, functional status,
cytological findings and malignancy risk. Benign, asymptomatic nodules without
compressive features are typically managed with observation and periodic
ultrasound monitoring4. In cases
of nodular hyperfunction, such as toxic adenomas or multinodular goiter,
treatment options include radioactive iodine therapy, antithyroid medications
or surgery, depending on symptom severity, patient age and comorbidities5. Surgical intervention, typically via
lobectomy or total thyroidectomy, is recommended for nodules with suspicious
cytology, rapid growth or confirmed malignancy6.
Minimally invasive techniques such as ultrasound-guided PEI or RFA are
alternatives for patients with symptomatic benign nodules, toxic nodules, some
papillary thyroid cancers and for patients who are poor surgical candidates or
wish to avoid surgery7. The
therapeutic approach must be individualized, weighing the risks and benefits of
each modality within the context of the patient’s overall health, nodule
characteristics and preferences.
Non-surgical
options for managing benign thyroid nodules have gained increasing attention as
effective and less invasive alternatives to thyroidectomy, particularly in
patients seeking to preserve thyroid function and avoid surgical risks. These
approaches have demonstrated substantial efficacy in reducing nodule volume and
alleviating compressive symptoms. Such interventions are especially valuable in
treating cystic or solid nodules that are symptomatic or cosmetically
concerning but histologically benign. Compared to surgery, these techniques
offer the advantages of minimal downtime, low complication rates and
cost-effectiveness, aligning with current trends toward precision and
personalized thyroid care8.
PEI
is a minimally invasive, ultrasound-guided treatment used primarily for benign
cystic or predominantly cystic thyroid nodules. The procedure involves
injecting 95-99% ethanol directly into the nodule to induce cellular
dehydration, coagulative necrosis and vascular thrombosis, leading to volume
reduction and symptomatic relief9.
PEI is particularly effective for recurrent thyroid cysts that reaccumulate
fluid after aspiration, with reported volume reductions of up to 85–90% and low
recurrence rates10. Compared to
surgery, PEI offers advantages such as preservation of thyroid function,
minimal risk of complications and reduced healthcare costs. However, its
efficacy in solid or malignant nodules is limited and multiple sessions may be
required for optimal outcomes. Complications are generally rare and mild,
including transient pain, voice changes or local inflammation.
RFA
is an image-guided, minimally invasive procedure increasingly used for the
treatment of benign thyroid nodules, particularly those causing compressive
symptoms or cosmetic concerns. It involves the application of high frequency
alternating current via an electrode to generate localized heat, inducing
thermal coagulative necrosis and progressive shrinkage of nodule tissue. RFA
has demonstrated excellent efficacy in reducing nodule volume-typically by 50-90%
over 6-12 months-with significant improvements in symptom and cosmetic scores11. Unlike surgical resection, RFA preserves
thyroid function, avoids general anesthesia and is associated with a low risk
of complications, such as transient voice changes or hematoma. It is now
endorsed by international guidelines, including the Korean Society of Thyroid
Radiology and the European Thyroid Association, as a first-line treatment for
appropriate benign nodules12.
Ongoing research is also exploring its role in selected low-risk papillary
thyroid microcarcinomas.
The
combined use of PEI and RFA has emerged as a promising strategy for the
management of complex thyroid nodules, particularly those with both solid and
cystic components or those that are partially recurrent after single-modality
treatment13. PEI is highly
effective for aspirating and sclerosing cystic portions of nodules, while RFA
is better suited for ablating solid tissue. When used sequentially-typically
with PEI applied first to manage the cystic part followed by RFA for the solid
portion-the combined approach enhances overall volume reduction, minimizes
recurrence and improves symptom and cosmetic outcomes14. Studies have shown that this synergistic
technique can achieve greater efficacy than either modality alone, particularly
for predominantly cystic nodules with residual solid tissue15. Additionally, the combination may help
avoid surgery in selected patients, preserving thyroid function, reducing the
risk of complications and increasing patient satisfaction. Microwave ablation
(MWA) shows equally effective results in similar cases and could be an
alternative to RFA16. Although in
this case study, RFA was only performed on one occasion, this patient’s success
demonstrates the additive benefits of PEI with RFA over time in challenging
nodules.
Learning
points
Combination therapy enhances efficacy in
complex nodules: Using RFA
and PEI in tandem can be especially beneficial for large, mostly cystic or
recurrent thyroid nodules that do not respond well to PEI alone. PEI targets
the cystic component effectively, while RFA ablates the solid portion, offering
a more complete and sustained reduction in nodule volume.
Minimally invasive alternatives reduce surgical
burden: For patients who are
poor surgical candidates or prefer non-surgical approaches, the combined use of
PEI and RFA provides a safe, outpatient-based solution with fewer
complications, quicker recovery and preservation of thyroid function.
Treatment must be individualized based on
nodule composition and recurrence: Assessment
of the nodule’s size, cystic-to-solid ratio and prior treatment response is
critical in planning a tailored approach. This case highlights the importance
of adapting the treatment modality to optimize long-term outcomes and minimize
recurrence.
Acknowledgments
None.
Contributors
Angela D Mazza is the only contributor to the
management of this patient and manuscript submission.
Funding
No public or commercial funding.
Disclosures
None declared.
Informed
Patient Consent for Publication
Signed informed consent was obtained directly
from the patient.
References
5. Ross DS. Radioiodine therapy for
hyperthyroidism. N Engl J Med 2011;364(6):542-550.