Continuous Erector Spinae Plane Analgesia Covering Cervico-Thoracic and Lumbo-Sacral Dermatomes in a 19-month-old child following Excision of Severe Post Burn Contracture and Extensive Skin Grafting: Case Report
Abstract
Post-burn scar excision and split-skin grafting is
known to produce severe postoperative pain and is the most distressing symptom
reported by patients in the early postoperative period. Erector spinae plane
block is a recently described analgesic technique. We present the effective use
of continuous erector spinae plane analgesia in a nineteen-month-old child with
severe post burns scarring who underwent extensive plastic surgery involving 16
dermatomes including cervico-thoracic and lumbo-sacral dermatomes. We conclude
that erector spinae plane analgesia has the potential for widespread use in the
pediatric population.
Keywords: Erector spinae plane analgesia; Burns; Skin grafting
Case Presentation
A
nineteen-month-old male child weighing nine kilogram was admitted with severe
post burn injury involving the face, chest wall, axilla and entire upper limb
on the left side. There was severe post burn contracture at the axilla, elbow
and fingers. The child was scheduled for excision of the contractures with
split-skin grafting. The child appeared severely traumatized by the burn injury
that occurred three months prior to the admission. He was extremely anxious and
distressed at the pre-anesthetic assessment.
Informed
written parental consent was taken for insertion of the erector spinae plane
catheters. Additional parental consent was obtained for deidentified data
including photographs to be used for publication in a peer reviewed journal.
The
child underwent general anesthesia and the trachea was intubated. Anesthesia
was maintained with oxygen, nitrous oxide and isoflurane. Muscle relaxation was
maintained with atracurium. Intraoperative analgesia included intravenous
fentanyl (3 microgram/kg), intravenous paracetamol (15 mg/kg) and per-rectal
diclofenac (25 mg). The child underwent extensive excision of the contracture
involving the left chest wall, axilla, arm and fingers. Skin graft was taken
from the left thigh circumferentially and posterior aspect of the leg (Figure
1). A total of 16 dermatomes were involved that included cervical C4 to
thoracic T4 (upper limb and chest wall) and lumbar L2 - sacral S3 (lower limb).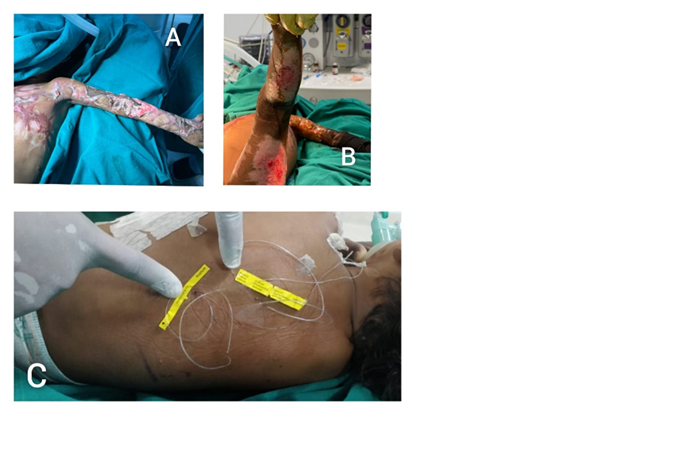
Figure
1: Image A shows the extent of post burn injury affecting the left chest
wall, axilla and upper limb on day 18 following surgery. Image B shows the
split skin graft donor sites in the left lower limb. Image C shows the two
subcutaneously tunnelled erector spinae catheters at thoracic T2 and lumbar L2
levels
On
completion of the surgical procedure, the child was positioned prone and two
erector spinae plane (ESP) catheters were sited under real-time ultrasound
guidance1. The first catheter was inserted at T2 level in the caudo-cranial
direction using an 18-gauge Tuohy needle and 5 cm of a 20-gauge catheter
(Perifix® Complete Set, B. Braun SE, Carl-Braun-Straße 1, 34212 Melsungen,
Hessen, Germany) was inserted in the plane after saline hydrodissection1. The
second catheter was placed at lumbar L2 level in a cranio-caudad direction and
5 cm of the catheter was placed in the plane. Both catheters were
subcutaneously tunneled and secured (Figure 1). A mixture of bupivacaine (25
mg), dexamethasone (1 mg) and dexmedetomidine (3 microgram/kg) diluted to 20 mL
was equally divided and injected into each catheter. Postoperative analgesia
was maintained with 8 hourly top-ups (10 mg bupivacaine diluted to 10 ml per
catheter) and regular acetaminophen (20 mg/kg). Rescue analgesia included
intravenous tramadol and per rectal diclofenac.
The
ESP catheters were topped-up for four days postoperatively. The child remained
comfortable during the postoperative period requiring just one dose each of
intravenous tramadol (2 mg/kg) and per-rectal diclofenac (25 mg) on the first
day. Breakthrough pain was caused by a delay in topping-up the ESP catheters.
The catheters were left in-situ and were used to provide analgesia on day 7
following further debridement and change of dressing. The catheters were
removed on day 9. The child had an uneventful recovery and was discharged on
day 18. There was no complication related to prolonged ESP catheter placement.
Discussion
The authors present the first case of
continuous ESP analgesia covering concomitant cervico-thoracic and lumbo-sacral
dermatomes in a paediatric patient following extensive plastic surgery. ESP
analgesia has been reported for thoracic, abdominal and lower limb surgeries in
children covering thoracic T1-lumbar L4 dermatomes1,2.
However, to the best of our knowledge, this is the first report where ESP
analgesia was used to provide widespread analgesic cover for nociceptive pain
arising from 16 dermatomes including cervical, thoracic, lumbar and sacral
dermatomes. Local anaesthetic deposition in the ES plane produces analgesia by
blocking the paravertebral nerves3.
The sympathetic block and vasodilatation observed following ESP block could be
beneficial in enhancing healing post skin grafting4. In addition, the technique
has an excellent safety profile4,2,3,5.
Split-skin grafting is known to produce severe
postoperative pain and donor site pain is one of the most distressing symptoms
reported by patients in the early postoperative period6. Postoperative analgesic techniques
recommended include continuous subcutaneous infusion of local anaesthesia
(CSLA), subcutaneous local anaesthetic injections, topical application of local
anaesthetic (LA) medication in wound dressing and pharmacological medications7. Subcutaneous LA injections, CSLA or
topical LA applications were not feasible options or this child. As
postoperative pain after split-skin grafting is primarily nociceptive in
nature, pharmacological agents including opioids have poor efficacy. In a child
with extensive surgical trauma, postoperative analgesia would have been a
challenge especially considering the severe psychological impact from the burn
injury.
The authors are aware of the major limitations
of anecdotal reports. We did not perform formal paediatric pain assessments.
The child was severely traumatized and extremely anxious. On the preoperative
ward, the child was observed to be prone to uncontrollable crying during any
examination that produced pain. During the first 72 hours, the child had only
one episode of uncontrollable crying that coincided with delay in topping up
the ESP catheters.
We conclude that continuous erector spinae
plane analgesia has the potential for widespread use in the paediatric
population.
Disclosures
No conflicts of interest declared
Funding
None declared
References