Cystic Metastasis of Papillary Thyroid Microcarcinoma in Acromegalic
Abstract
Microcarcinoma
is defined as a tumor less than or equal to 1 cm and represents an indolent
pathology with very low mortality, when it comes to classic papillary
carcinoma. The appearance of metastases in neck ganglion chains is relatively
frequent, they are generally micro metastasis, but sometimes they can be
larger. In the general population, the secondary lymph node in these cases does
not change mortality, but if it is associated with certain diseases such as
acromegaly, the prognosis may be somewhat bleaker. We present the case of a
patient whose diagnosis of papillary carcinoma comes through a cystic lymph
node metastasis almost six times larger than the size of the neoplasm that
originated it.
Keywords: Microcarcinoma; Indolent
pathology; Ganglion chains; Papillary Carcinoma
Introduction
Acromegaly
is a rare disease caused by sustained hypersecretion of growth hormone (GH),
usually caused by a pituitary tumor. It produces concomitant elevation of
insulin-like growth factor type 1 (IGF-1). A population prevalence of up to
1000 per million individuals is suggested1. It is associated with
premature mortality from cardiovascular disease and the development of benign
and malignant tumors. IGF-1 is proposed to play an important role in thyroid
growth and the genesis of goiter. The thyroid size measured with ultrasound is
larger than in the normal population, depending on the evolution of the
disease.
Differentiated
thyroid cancer (CDT) is the most prevalent thyroid cancer and is among the most
commonly diagnosed cancers in the United States2. The prevalence of this
type of tumor is slightly elevated in patients with acromegaly. Prolonged
stimulation of the thyroid follicle by GH/IGF-1 induces both enlargement and
hyperactivity and nodule formation, therefore, multinodular goiter is a common
finding. The chance of nodules increases with disease progression and IGF-1
values. In a systematic review, 4% of patients with acromegaly also had thyroid
cancer, which is higher rates than for the general population3.
Thyroid
function is usually normal, but some patients with goiter have subclinical
hyperthyroidism and a small amount of it has central hypothyroidism caused by
the pituitary tumor4.
Case Report
A 35-year-old man, heavy smoker, cognitive impairment and schizophrenia, with acromegaly of 10 years of evolution, who underwent 3 surgeries by sphenoidal transept and then treatment with octreotide 20 mg every 30 days for 6 months. He had been in remission for the past 4 years with IGF1: 81.9 ng/mL, which was normal for his age and sex. In the last MRI, asymmetrical remaining pituitary sun was observed at the expense of a depressed left lateral area with heterogeneous enhancement. He presented hypopituitarism and was substituted with prednisone 5mg/day, levothyroxine sodium 125 mcg/day and testosterone enanthate 250 mg every 21 days, intramuscularly. From the repercussions of his disease, he developed mild obstructive sleep apnea syndrome; in the cardiovascular area, he had an echocardiogram with mild biventricular and biauricular dilation, normal LVEF. Video colonoscopy was performed and showed hyperplastic polyps, without other lesions; Fibro gastroscopy showed no lesions. The examination highlights acromegalic facies, great magnification of supraciliary arches, diastema, wide, light hands and feet. Weight: 88 Kg Size: 189 cm. At the level of the neck, she presented palpable thyroid, without clearly delimiting nodules; Left mobile lower carotid adenopathy, approximately 4 cm. Increased dorsal kyphosis, dextro-convex scoliosis. Thyroid ultrasound showed thyroid volume of 14 cc, bilateral thyroid nodules, the largest on the left of 10 x 10 x 7 mm, poorly defined with microcalcifications and peripheral vascularization. At the left lower carotid jugular level, there is evidence of cystic image with echoes inside in relation to an already known brachial cyst, measuring 31 x 28 x 25 mm (L, T, AP) (Figure 1). It is noteworthy that when reviewing the previous history, it was found that the left cystic nodular lesion had at least 5 years of evolution, the follow-up was done with ultrasound and FNA on four occasions, it had maintained its size in that period of time and the reports were of brachial cyst, cystic tumor with macrophages, detritus and cholesterol crystals. The ultrasound-guided puncture of the left thyroid nodule was reiterated again, which reported colloid substance, small and medium-sized thyroid cells scattered and in plaques, with frequent micro and macrofollicular arrangement, it is classified as follicular lesion (Bethesda III). The puncture of the left tumor reported macrophages and plaques of epithelial cells, reminiscent of medium thyroid cells, with a moderate degree of anisocariosis, prominent nucleoli, some nuclear pseudo-inclusion and intense cytoplasmic vacuolization. Thyroglobulin by needle lavage was greater than 500 ng/ml. Cytologically: although the presence of a neoplastic nodule at the thyroid level could not be evidenced, the ultrasound, cytological and biochemical characteristics led to the suggestion of metastatic adenopathy of CDT. Because he is a young male patient, with a presumptive diagnosis of CDT lymph node metastasis, associated with acromegaly, which increases the risk of thyroid pathology, with a greater potential for nodule growth, it was decided to perform thyroidectomy. Surgery was performed without complications and the pathology reported: papillary carcinoma (PC), with conventional and follicular pattern of 7 mm major axis in the left lobe; it is intraparenchymal, does not involve the organ capsule (Figures 2 and 3). It associates adenomatoid nodular hyperplasia with Hürthlerian change. From recurrent dissection: 7 lymph nodes were obtained, of which 2 had PC micro metastasies. They measure 0.2 mm, one is capsular and the other subcapsular. From the low jugular-carotid ganglion: cystic metastasis of the PC, 41 mm major axis. The preserved lymph node parenchyma is referred to a small peripheral cap. He underwent 100 mCi of I131 with Thyrogen® for his secondary hypothyroidism, without complications and the dose of levothyroxine was subsequently increased to 150 mcg/day.
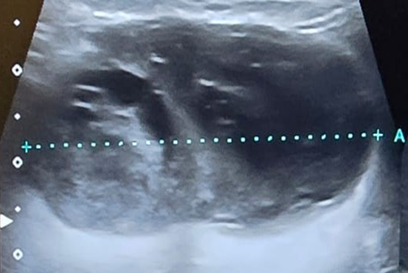
Figure 1: Thyroid ultrasound showed
the presence of a rounded lesion with irregular and poorly defined contours,
rounded morphology, heterogeneous echogenicity, with internal hyperechogenic
areas that could correspond to microcalcifications. The cystic component of the
lesion is observed in the dark sector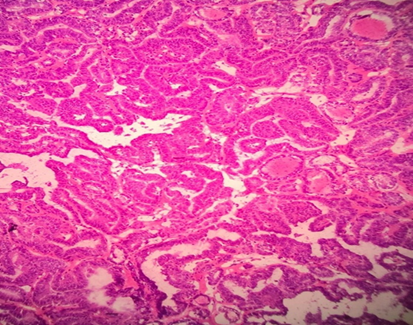
Figure 2: Pathology (H and E).
Micrograph showing an epithelial proliferation with a predominant papillary
pattern, fibrovascular projections covered by neoplastic cells. Areas with
complex follicular formations and patterns are also identified. The cells that
line the papillae have enlarged, oval nuclei with irregular margins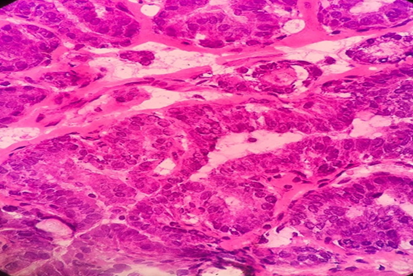
Figure 3: Pathology (H and E).
Micrograph at higher magnification where cells with optically clear or empty
nuclei are observed "frosted glass appearance". They have enlarged,
oval nuclei with nuclear clefts (grooves) and intranuclear pseudoinclusions, diagnostic
cytological features of papillary thyroid carcinoma
Discussion
Thyroid gland enlargement is described in patients with acromegaly
and can be diffuse or multinodular. There was a report that showed that of 37
acromegalic patients, 92% had an increased thyroid by ultrasound; The mean
thyroid size was more than five times normal5. Another found that 87% had palpable diffuse or multinodular
goiter6.
Long-term excess GH-IGF1 causes overgrowth of tissues, such as
connective, cartilage, bone, skin and organ meats. Other systemic complications
include cardiovascular disease, sleep apnea, metabolic disorders and colon
neoplasia4.
In addition to these patients' increased risk of colon polyps and
cancer, acromegaly may be associated with other tumors. In men, a greater
number of malignant tumors, such as adenocarcinomas of the colon, stomach,
esophagus and melanoma, were observed in a cohort of 1041 men with acromegaly
and increased frequency of thyroid cancers has also been reported7.
The annual incidence of CDT in the general population tripled from
4.9 per 100,000 in 1975 to 14.3 per 100,000 in 2015. Approximately 25% of new
thyroid cancers diagnosed between 1988 and 1989 were <1 cm, compared with
39% of new thyroid cancer diagnoses between 2008 and 20092,8.
PC is typically indolent and is associated with long-term survival
of 96% at 5 years, 93% at 10 years and more than 90% at 20 years. Overall, PC
mortality rates are 1% to 6.5%, with an overall recurrence rate of 15% to 35%;
Tumor recurrence usually occurs in the tumor bed, cervical lymph nodes or more
rarely at distant sites2,9,10.
However, the evolution with acromegaly can be more torpid and
these patients have cancers as the third cause of death. These include those of
the colon, prostate, but thyroid may be the most common malignancy associated
with the disease11. IGF-I may promote tumor progression and perhaps facilitate
neoplastic initiation12.
Several studies have shown a positive correlation between thyroid
volume and serum IGF-I concentration13.
Another study showed no correlation between goiter and IGF1
levels. It was described that patients with secondary hypothyroidism had a
thyroid volume twice as small. Goiter was diagnosed in 87% of patients,
including diffuse (17.1%) and nodular (69.9%) goiter, with no significant
differences between patients with active or controlled disease or among those
with secondary hypothyroidism14.
Although goiter occurs with high frequency in patients with
acromegaly, it is not yet clear whether normalization of IGF-1 levels could
decrease it. However, it has been reported that the increase in thyroid volume
associated with acromegaly, but not nodular goiter, could be reversed in cured
acromegaly15.
Active surveillance in low-risk papillary thyroid microcarcinomas
should be the first-line management modality, because only a small percentage
of low-risk patients progress (10-15%)16; this was not the case in our patient, so it was not considered.
Regarding the microcarcinoma that occurred in this case, it has
been documented that multifocality and extracapsular invasion of papillary
thyroid microcarcinoma (PTCM) are associated with the presence of metastatic
adenopathy. But it was not the case that there was only one focus despite the
large metastatic size. Metastatic PCM, with more aggressive treatments, has an
excellent long-term prognosis17.
The presence of metastatic adenopathy in papillary carcinoma is a
factor associated with recurrences18.
PC lymph node metastases may appear as solid or cystic masses.
When they are solid, they are usually not a diagnostic problem, but solitary
cystic lymph node metastases could be misinterpreted as a benign cervical
cystic mass. In one study19 conducted for most cystic metastases, they were ipsilateral to
the primary tumor (87.8%) and were located in the middle or inferior jugular
chain (73.2%). In 14.9% of cases, cystic metastases in the lymph nodes were the
initial manifestation of the disease. Only 6.2% of all lymph node metastases
were purely cystic (all of these occurred in patients younger than 35 years). This
study concludes that in most patients, cystic lymph node metastases are
characterized by ultrasound by having a thickened external wall, internal
echoes, internal nodularity and septa (as happened in this case). However, in
younger patients, the lymph nodes may present a purely cystic appearance,
simulate gill cysts and thus require biopsy for definitive diagnosis and
treatment planning. This patient spent several years with punctures in what was
said to be a brachial cyst and it was the thyroglobulin needle washing that
alerted mainly that it corresponded to a metastasis19.
Cervical metastases due to carcinoma can produce subcortical
liquefaction resulting in a discrete fluid-filled cervical mass. Diagnostic
procedures such as FNA, ultrasound, CT or MRI may fail to diagnose the nature
of these lateral cervical lesions. Excision of the cystic mass is often needed
to confirm the diagnosis20.
Reports suggest that the most common presentation of thyroid
cancers is a palpable thyroid nodule, but secondary lymph nodes in the neck
appear in 20 to 70% of cases. Metastasis in cervical nodes as the first and
only manifestation of PC is uncommon. Cervical adenopathy as the only
presentation of metastatic thyroid carcinoma has been reported in up to 13.4%
by some series21.
Ultrasound features that suggest the presence of metastatic lymph nodes include
enlargement (this patient had years with the same size of adenopathy),
irregular borders, round shape, poorly defined contours, absence of echogenic
hilum, microcalcifications, cystic areas and hypervascularity8,9. Cystic
changes in the cervical lymph nodes are suggestive of metastatic PC22,23.
In our center, a study of microcarcinoma in 10 years was
published, we found that 83.3% did not have lymph node metastases and 14.3%
presented the diagnosis24.
Conclusion
The incidence of tumors is higher in patients with acromegaly,
both benign and malignant, being the third cause of death, after cardiovascular
and respiratory. The prevalence and mortality of the different tumors are
independent of the general population.
PC is the most common histological type in general and also
associated with GH hypersecretion.The follow-up of these patients is essential, since the risk of
developing cancer is directly proportional to the duration of the underlying
disease.
References
2. Ringel M, Sosa J, Baloch Z, et al. 2025 American Thyroid Association Management Guidelines for Adult Patients with Differentiated Thyroid Cancer. Thyroid 2025; 35(8):841-985
3. Wolinski K, Czarnywojtek A, Ruchala M. Risk of thyroid nodular disease and thyroid cancer in patients with acromegaly--meta-analysis and systematic review. PLoS One 2014;9(2):88787.
4. Melmed S, Katznelson L, Snyder P, Martin K. Causes and clinical manifestations of acromegaly 2025.
5. Cheung N, Boyages S. The thyroid gland in acromegaly: an ultrasonographic study. Clin Endocrinol (Oxf) 1997;46(5):545-549.
6. Kasagi K, Shimatsu A, Miyamoto S, Misaki T, Sakahara H, Konishi J. Goiter associated with acromegaly: sonographic and scintigraphic findings of the thyroid gland. Thyroid 1999; 9(8):791-796.
7. Gullu BE, Celik O, Gazioglu N, Kadioglu P. Thyroid cancer is the most common cancer associated with acromegaly. Pituitary 2010;13(3):242-248.
8. Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg 2014;140(4):317-322.
9. Haugen BR, Alexander EK, Bible KC, et al. American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016;26(1):1-133.
10. Kim K, Kim JK, Lee CR, et al. Comparison of long-termprognosis for differentiated thyroid cancer according to the7th and 8th editions of the AJCC/UICC TNM staging system. Ther Adv Endocrinol Metab 2020;11.
11. Gullu BE, Celik O, Gazioglu N, Kadioglu P. Thyroid cancer is the most common cancer associated with acromegaly. Pituitary 2010;13:242-248.
12. Loeper S, Ezzat S. Acromegaly: Rethinking cancer risk. Rev Endocrine Metab Disord. 2008;9:41-58.
13. Lewiński A, Marcinkowska M. Acromegaly and the thyroid gland. Thyroid Res 2015;8(1):1-4.
14. Natchev E, Vandeva S, Kovatcheva R, Kirilov G, Kalinov K, Zacharieva S. Thyroid gland changes in patients with acromegaly. Arch Endocrinol Metab. 2020;64(3):269-275
15. Chen Z, Jiang X, Feng Y, et al. Decrease in acromegaly associated thyroid enlargement after normalization of IGF1 levels: a prospective observation and in vitro study. Endocr Pract 2020;26(4):369-377.
16. Parada U, Elicegui V, Guarneri C, Mintegui G, Neirotti R. Papillary thyroid microcarcinoma: Active surveillance. Literature review. Rev Chil Endo Diab 2023;16(4):124-129.
17. Ruiz J, Rios A, Rodríguez J, Paredes M, Soriano V, Oviedo M, et al. Risk factors for lymph node metastases in papillary thyroid microcarcinoma. Cir esp 2020;98:219-225.
18. Ito Y, Miyauchi A, Kobayashi K, Kihara M, Miya A. Static and dynamic prognostic factors of papillary thyroid carcinoma. Endocr J 2014;61:1145.
19. Wunderbaldinger P, Harisinghani M, Hahn P, Daniels G, Turetschek K, Simeone J. Cystic lymph node metastasis Papillary thyroid carcinoma. AJR 2002;178:693-697.
20. Ramos M, Hassan H, Barrera J, et al. Cervical metastasis of papillary thyroid carcinoma. Rev Esp Cirug Oral and Max 2013;35(1):47-49.
21. Singh A, Butuc R, Lopez R. Metastatic papillary thyroid carcinoma with absence of tumor focus in thyroid gland. Am J Case Rep 2013;14:73-75.
22. Kessler A, Rappaport Y, Blank A, et al. Cystic appearance of cervical lymph nodes is characteristic of metastatic papillary thyroid carcinoma. J Clin Ultrasound 2003;31(1):21-25
23. García M, Valenzuela M, Fernández F. Lymph node metastasis as a presentation of a papillary carcinoma of the occult thyroid, follicular variety. Case report. Rev Chil Endo Diab 2021;14(2):77-80.