Early Pyogenic Granulomas in Older Adults treated with Topical Timolol: A Case Series
Abstract
Topical timolol has been employed to treat pyogenic
granulomas (PG) in children and young adults with mixed results. To date, there
are no studies examining the use of topical timolol in older adults
(middle-aged and elderly age groups) with primary PG. We report a series of 5
patients (age range 42-87 years) with early PG who responded favourably to
topical timolol.
Keywords:
Pyogenic granuloma; Adult; Elderly; Topical timolol
Introduction
Topical timolol is a
beta-adrenergic receptor antagonist that has been employed in the treatment of
pyogenic granulomas (PG) due to its vasoconstrictive and anti-angiogenic
properties. Patients who are not surgical candidates, or who have lesions over
delicate areas – where invasive modalities are not desirable – may benefit from
topical timolol as a therapeutic option. Most studies examining the use of
topical timolol in the treatment of PG have been undertaken amongst children
and young adults. Results have been variable across these studies. We report a
series of 5 adult patients (age range 42-87 years) with early PG (i.e. onset
1-4 weeks) who responded favourably to topical timolol (Table 1).
Table 1: Case
series of 5 adults with pyogenic granulomas treated with topical timolol M:
male, F: female
|
Case |
Age/race/sex |
Co-morbidities |
Site |
Duration of lesion |
Size (mm) |
Treatment |
Result (at 4 weeks) |
|
1 |
55/Chinese/M |
None |
Right middle finger |
4 weeks |
6x6 |
Topical timolol 0.5% 2 drops
QDS |
PR |
|
2 |
68/Chinese/F |
Hyperlipidaemia |
Left ring finger |
2 weeks |
3x2 |
Topical timolol 0.5% 2 drops
QDS |
CR* |
|
3 |
58/Chinese/F |
Diabetes, hyperlipidaemia,
fibroids |
Umbilicus |
1 week |
7x8 |
Silver nitrate, followed by
topical timolol 0.5% 2 drops BD |
CR** |
|
4 |
42/Indian/M |
None |
Left big toe |
4 weeks |
5x7 |
Cryotherapy, followed by
topical timolol 0.5% 2 drops BD |
PR*** |
|
5 |
87/Chinese/M |
Hypertension, IHD, COPD/asthma BPH |
Left wrist |
1 week |
6x6 |
Cryotherapy, followed by
topical timolol 0.5% 2 drops QDS |
CR |
CR: complete response –
total disappearance of the lesion, PR: partial response – reduction in the
number and/or size of the lesions/ decrease in bleeding tendency,
COPD:
Chronic obstructive pulmonary disease, IHD: Ischaemic heart disease, BPH:
Benign prostatic hyperplasia
*CR
at 1 week
**CR
at 3 weeks
***achieved
CR at 11 weeks
Case
1
A
55-year-old Chinese male presented with a growth over his right middle finger
that bled intermittently over 4 weeks. Examination showed a 6mm x 6mm friable
vascular papule clinically consistent with PG (Figure 1a).
He received treatment with topical timolol 0.5% 2 drops 4 times daily. A
decrease in the size of the lesion and resolution of bleeding was noted 4 weeks
later (Figure 1b).
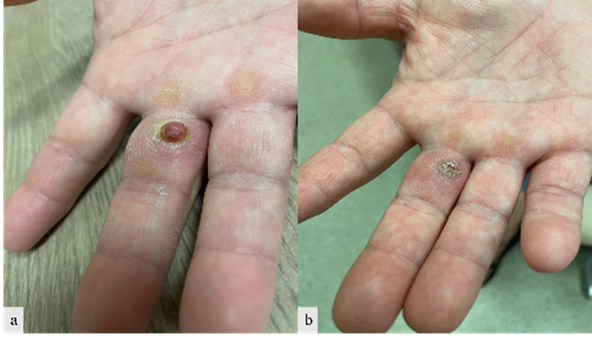
Figure 1a: Before
timolol1 1b: Decrease in size and resolution of
bleeding after timolol
Case
2
A
68-year-old Chinese female presented with a growth over her left ring finger
after accidentally scraping it against a metal chair 2 weeks ago. The lesion
bled intermittently on contact. Examination showed a 3mm x 2mm friable vascular
papule clinically consistent with PG (Figure 2a). She received
treatment with topical timolol 0.5% 2 drops 4 times daily. The lesion resolved
within 1 week (Figure 2b).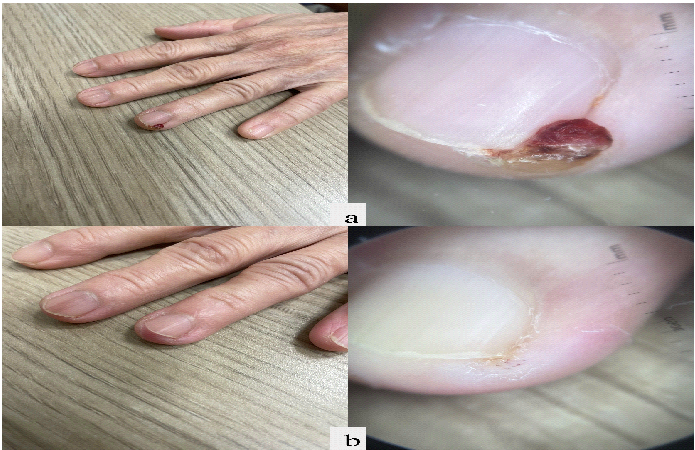
Figure 2a:
Before timolol 2b: Resolution of lesion after timolol
at 1 week
Case 3
A
58-year-old Chinese female presented with a growth over the umbilicus with
occasional bleeding over 1 week. Examination showed a 7mm x 8mm friable
vascular papule clinically consistent with PG (Figure 3a).
She received treatment with a single application of topical silver nitrate,
followed by topical timolol 0.5% 2 drops twice daily. The lesion resolved in 3
weeks (Figure 3b).
Figure 3a: Before
timolol 3b: Resolution of lesion after timolol
at 3 weeks
Case 4
A 42-year-old Indian male presented with a growth over the left big toe that bled intermittently over 4 weeks. Examination showed a 5mm x 7mm friable vascular papule with contact bleeding, clinically consistent with PG (Figure 4a). He received treatment with a single cryotherapy session, followed by topical timolol 0.5% 2 drops twice daily. A reduction in the size and bleeding tendency of the lesion was noted 4 weeks later (Figure 4b), and complete resolution was seen at 11 weeks (Figure 4c).
Figure 4a:
Before timolol 4b: Reduction in the
size and bleeding tendency after timolol at 4 weeks 4c: Resolution of the lesion after timolol at 11 weeks
Case
5
An
87-year-old Chinese male presented with a growth over his left wrist that bled
intermittently over 1 week. Examination showed a 6mm x 6mm friable vascular
papule clinically consistent with PG
(Figure 5a). He received treatment
with a single cryotherapy session, followed by topical timolol 0.5% 2 drops 4
times daily. The lesion resolved in 4 weeks (Figure 5b).
Figure
5a: Before timolol 5b: Resolution of lesion after timolol
at 4 weeks
Discussion
The lack of uniform clinical response to
topical timolol has been thought to be due to the expression of only 50% of beta-adrenergic
receptors in PG1. Amongst various factors influencing
clinical response, a younger age was the only factor found to predict a more
favorable outcome2. The affinity of beta-adrenergic receptors
to their ligands decreases as a person ages, with subsequent reduction in their
binding sensitivity. Theoretically, beta-blockers would be of less value in
treating PG in older patients3.
Topical timolol in the treatment of PG in
children is well-described in existing literature. Among adults, most studies
to date have been performed in the younger age group (Table 2).
Table
2. Studies examining the use of topical
timolol in adult patients with pyogenic granulomas.
|
Study, year |
n |
Age (mean) |
Timolol (%) |
Duration of treatment
|
Result |
Remarks |
|
Millsop J et al., 2014 [9] |
1 |
39 |
0.5 solution once daily |
3 months |
CR |
Topical timolol was combined
with intralesional steroids and laser |
|
Gupta D et al., 2016 [10] |
10 |
24.9 |
0.5 solution four times a
day |
3-24 days |
4 CR, 3 PR, 3 NR |
The oldest patient was a
50-year-old male with multiple scalp PGs - CR for smaller lesions but NR for
all other lesions. |
|
El Taweel AEI et al., 2020
[2] |
10 |
28.1 |
0.5 cream twice daily |
2 months |
2 CR |
Among the studied variables,
age was the only factor influencing clinical response. Younger patients
responded better. |
|
Williams N and Morrison B
2020 [11] |
1 |
62 |
0.5 solution twice daily |
10 weeks |
CR |
Topical timolol was combined
with topical steroid/topical antifungal |
|
Patra AC et al., 2022 [12] |
22 |
28.6 |
0.5 solution twice daily |
6 weeks |
2 CR, 20 PR |
Percentage size reduction:
40.9% with topical timolol versus 3.39% with placebo, p = 0.002 |
|
Manjeet et al., 2023 [13] |
12 |
25 |
0.5 solution twice daily |
4 weeks |
2 CR, 5 PR, 5 NR |
The oldest patient was a
50-year-old male with a right index finger PG who showed NR at 4 weeks. |
CR: complete response – total disappearance of the lesion, PR: partial response – reduction in the number and/or size of the lesions/ decrease in bleeding tendency, NR: no response – absence of clinical response
PG: pyogenic
granuloma
There
have been few studies examining the use of topical timolol in older adults –
these were conducted in patients with paronychia and/or pyogenic granuloma-like
lesions secondary to epidermal growth factor receptor inhibitor therapy, rather
than isolated primary PG lesions4-6.
Our
study supplements current literature by looking specifically at the response
amongst older adults who fall into the middle-aged (40-59 years) and elderly
(≥60 years) age groups. We report 2 women and 3 men (age range: 42-87 years,
mean: 62 years) who received treatment with topical timolol for PG. All
patients responded to topical timolol by the 4 week mark. Complete response was
seen in 3 patients within 1 to 3 weeks. These results are surprisingly
favourable, considering previous studies which
have suggested that topical beta-blockers would be less effective in older
patients. We postulate that the encouraging response seen in our study may be
due to the selection of patients with early PG (duration of lesions: 1-4
weeks). Early PG tend to have a greater vascular component, compared to later
ones which consist of a larger fibrous component7,8.
Given that topical timolol exerts its therapeutic effects on the vascular
component, it is logical that patients with early PG tend to respond better.
This
study is subject to certain limitations. All lesions were diagnosed clinically
without histological confirmation. Two patients received cryotherapy and 1
patient received topical silver nitrate application in addition to topical
timolol. Larger studies are needed to determine the efficacy of topical timolol
as monotherapy in this population, and longer term follow-up will be useful to
monitor for recurrence9-13.
Conclusions
Existing
literature supports the use of topical timolol in the treatment of PG in
children and young adults, and a younger age generally portends better
outcomes. Our study adds that topical timolol could also be efficacious in
older adults, if they have early PG. The age of the lesion may be as important
a factor as the age of the patient in predicting treatment outcomes.
References