Intrahepatic Subcapsular Hematoma Following Laparoscopic Cholecystectomy: A Case Report and Literature Review
Abstract
Background
Laparoscopic cholecystectomy (LC) is the gold standard
treatment for symptomatic gallstones, with an overall morbidity rate of less
than 7%. However, rare but potentially lifethreatening complications can occur,
such as intrahepatic subcapsular hematoma (ISH), which is reported in less than
1% of cases.
Case Report
We report the case of A 30-year-old woman with no
prior medical history, who underwent LC two months after an episode of
gallstone-induced acute pancreatitis. She was discharged the day after surgery
but returned on postoperative day two for a subcapsular hematoma. CT scan
showed an ISH with no evidence of any intra-abdominal haemorrhage. Since the
patient was stable, we opted for serial monitoring in the ICU and conservative
treatment. the patient was discharged the third day with no further complications.
Conclusion
ISH is a very rare but potentially life-threatening
complication following laparoscopic cholecystectomy. This case highlights the
importance of considering this uncommon condition in patients experiencing
abdominal pain after LC, emphasizing that prompt and accurate diagnosis and
treatment are essential for patient survival.
Keywords: Subcapsular liver hematoma; Laparoscopic
cholecystectomy; Complication
Introduction
Since
the first surgical removal of the gallbladder performed in the second half of
the 19th century, laparoscopic cholecystectomy (LC) remains the gold standard
treatment for symptomatic cholecystolithiasis patients with an overall
morbidity of less than 7%1-3.
Complications
of LC include iatrogenic bile duct injury, postoperative bleeding, bowel
injuries and infections. Intrahepatic subcapsular hematoma (ISH) is a rare
complication following LC occurring in less than 1%, however it can prove to be
life-threatening2-4.
Case Report
We present the case of a 30-year-old female,
with no medical history, such as systemic disease or any recent prescription,
who underwent a vaginal delivery 6 months ago and presented a gallstone acute
pancreatitis (Figure 1) 2 months prior to a laparoscopic cholecystectomy
(LC) (Figure 2).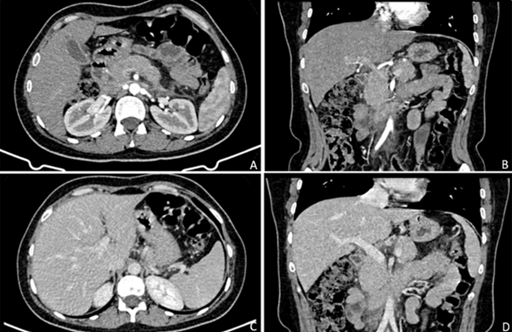
Figure
1: Pre-operative CT scan showing an acute pancreatis. No angioma, tumor or
vascular malformation were apparent
(A)
Arterial phase axial maximum intensity projection; (B) Arterial phase coronal
maximum intensity projection; (C) Portal venous phase axial maximum intensity
projection ; (D) Portal venous phase coronal maximum intensity projection
The patient was discharged at post-operative
day one, however on the second day after surgery, she presented to our
department with severe abdominal pain. Physical examination revealed a
tenderness in the right hypochondrium, hypotension and tachycardia at 130 beats
per minute.
We performed biological tests, that showed a
severe anemia with hemoglobin levels at 5g/Dl. Platelet count and coagulation
profile were within the normal range.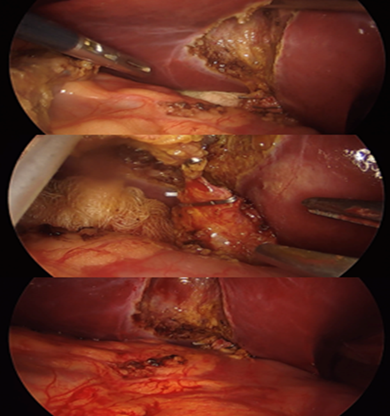
Figure 2: Per-operative view of laparoscopic cholecystectomy. No
complications or adverse event were observed intra-operatively
The patient underwent an abdominopelvic CT scan
which revealed a large subcapsular hematoma surrounding the lateral surface of
the right lobe, the hepatic artery, portal vein and hepatic veins opacified
normally and no contrast extravasation was visualized.
The patient was monitored in the UCI and after
being transfused, she stabilized, which prompted monitoring and surgical
abstention.
The patient was discharged on the third day
upon stabilization with no further complications (Figure 3).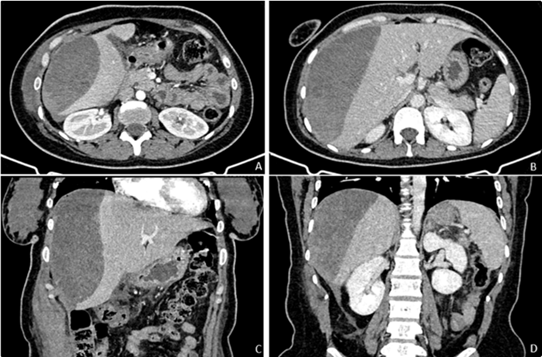
Figure
3: post-operative CT scan showing a subcapsular hematoma surrounding the
lateral surface of the right hemi liver, with no active bleeding or ruptured
capsule
(A)
Arterial phase axial maximum intensity projection; (B) Portal venous phase
axial maximum intensity projection ; (C+D) Portal venous phase coronal maximum
intensity projection
Discussion
LC is considered a safe procedure with an
overall morbidity of less than 7% in large cohort studies. Complications after
laparoscopic cholecystectomy occur in 2–6% of patients and bleeding is observed
in less than 1% of cases. The most frequent sites of bleeding after
laparoscopic cholecystectomy (LC) include the gallbladder bed, cystic artery,
trocar insertion points, falciform ligament and liver capsule tears. Although
intrahepatic subcapsular hematoma (ISH) is a rare complication following LC, it
poses a serious risk due to the potential for rupture and resulting hemodynamic
instability. When rupture occurs into the peritoneal cavity, the associated
mortality rate can reach 75%. These hematomas are typically found on the right
side of the liver. (in 75% of cases)1,2,5,6.
ISH may occur early, up to 24 hours after
surgery, as well as late, several weeks after the procedure1,7.
Some contributing factors have been described,
including iatrogenic injuries of the liver parenchyma and capsular tears,
during gallbladder traction or due to trocar placement. The presence of a
pre-operative pseudoaneurysm or a hepatic haemangioma that could be injured
during the procedure. Perioperative administration of nonsteroidal
anti-inflammatory drugs (NSAID) was reported in a number of cases of ISH
following LC with special emphasis on ketorolac use as it was associated with
the highest risk estimate of bleeding. The consumption of NSAIDs in the
postoperative period has also been proposed as an associated cause, since in
several cases the patient used ketorolac (up to 58.8%) or parecoxib in the
postoperative period. It has also been associated with anticoagulant therapy2,8,9.
Our patient, had no specific underlying cause,
as she had no coagulation disorders nor she was taking anticoagulants or
antiplatelet therapy. Furthermore, there was no bleeding source identified nor
a liver parenchymal injury identified throughout the surgery. there was also no
evidence of any hepatic haemangiomas, adenoma or tumour in the preoperative CT
scan performed 2 months prior to the LC. As a matter of fact, there are some
cases where the cause of post cholecystectomy ISH remains unexplained2,3.
16 cases of ISH after LC were reported from
1994 to 2015. Nearly half of the patients presented a hemodynamic instability.
All reported cases involved female patients, with ages ranging from 25 to 78
years. The majority of hematomas were located in the right hepatic lobe, with
some extending into the left lobe. At the time of diagnosis, only one case had
ruptured. Hepatic capsule laceration was found in two cases, one of whom also
took NSAIDS for pain management, Notably, 35.3% of the patients had no identifiable
risk factors3.
Patients with ISH can present in the
postoperative course with right upper quadrant abdominal pain, nausea, fever,
hypotension and tachycardia that does not improve with the administration of
intravenous fluids. Patients may also present with hemodynamic instability if a
rupture of the ISH has occurred with intraabdominal bleeding. Furthermore, an
infected hematoma may occur whereby the patient may present with fever,
abdominal pain or some features of sepsis. The time of occurrence in the
previously reported cases varies between 7 hours and 6 weeks of the
postoperative course. On ultrasound or CT scan, it appears as a collection of
fluid between the fibrous and serous layer of the liver2,8,9.
Depending on the patient’s symptoms and
condition, different therapy can be introduced from expectant management to
emergency surgical treatment1.
When the ISH is small, it is usually
asymptomatic, however, if it keeps growing, some complications may occur3.
The management of large ISH remains unclear,
however several strategies have been proposed, such as conservative management
with strict clinical observation, surgical management (laparotomy or
laparoscopy), percutaneous drainage or endovascular embolization. The choice is
conditioned by the patient’s clinical status, the size and cause of the
hematoma2,8.
As there is no clear management pattern because
of the few clinical cases reported, some authors proposed a conservative
treatment for two patients who developed a delayed ISH with fever. One patient
underwent computed-tomography-guided drainage and the other was managed
conservatively without any surgical or radiological procedure10,12-14.
Another author proposed a relaparoscopy for a
hemodynamically unstable patient who had a ruptured ISH with active bleeding
which was evacuated and controlled laparoscopically. One patient underwent
emergency laparotomy, evacuation and drainage of the ISH, which was probably
caused by an instrumental stab wound during LC10,14,15.
When an intrahepatic subcapsular hematoma (ISH)
is small, confined beneath the hepatic capsule and not associated with
intra-abdominal bleeding, conservative management is typically the preferred
approach. This involves careful monitoring of the hematoma over time. If the
hematoma becomes infected, percutaneous drainage under CT or ultrasound guidance,
along with appropriate antibiotic therapy, is the treatment of choice. In cases
involving a ruptured aneurysm, hepatic adenoma or angioma, selective embolization
of the bleeding vessel may be considered. More invasive interventions, such as
relaparotomy or relaparoscopy, may be necessary in the presence of hemodynamic
instability or rupture of the hematoma, particularly when associated with an
underlying hepatic tumor2,3,5,9.
Summary/Conclusion
ISH is an extremely rare but life-threatening
complication following LC. This case demonstrates the necessity of monitoring
patients who undergo LC and considering the possibility of ISH, although being
rare, in those who experience refractory postoperative hypotension. There is
still no universally accepted theory regarding the cause, treatment and
outcomes of this rare entity.
Consent
Written Informed consent was obtained from the
patient for the publication of her case as a report and was documented in the
patient’s medical notes. A copy of the written informed consent would be
available for review by the editor-in-chief of the journal on request.
Conflicts of Interest
The authors declare that there are no conflicts
of interest regarding the publication of this case report.
References
2. Eltaib Saad LO. Giant
Intrahepatic Subcapsular Haematoma: A Rare Complication following Laparoscopic
Cholecystectomy-A Case Report and Literature Review. Case Reports in Surgery
2020.