Multimodal Musculoskeletal Treatment in Refractory Chronic Headache: A Case Report
Abstract
Patients with chronic headaches frequently experience disabling
symptoms that heavily impact their quality of life and ability to perform
activities of daily living. Current standard treatment focuses on pharmacologic
interventions and includes abortive therapies such as analgesics and
migraine-targeting therapies. We report a case of a 66-year-old female with a
12-month history of a persistent, refractory secondary headache characterized
by cervicogenic and occipital neuralgia features, unresponsive to multiple
pharmacologic and non-pharmacologic interventions. After little progress was
made with her previous treatment plan of analgesics, Rimegepant (Nurtec),
physical therapy and dry needling, the patient was offered a multimodal
musculoskeletal approach, including acupuncture, osteopathic manual therapy
(OMT) and home exercise recommendations by a single physician provider. These
therapies have been shown to provide relief in patients suffering from chronic
pain. Following this multimodal approach, the patient reported significant
symptom relief in their headache frequency and intensity, allowing her to have
less reliance on medication, while also significantly improving her sleep
quality. This case demonstrates a potential avenue for further research to hopefully
develop new minimally invasive treatments of chronic headaches that can improve
a patient’s quality of life.
Keywords: Chronic headache; Multimodal musculoskeletal treatment;
Alternative medicine
Introduction
Chronic headaches are characterized by recurrent headaches occurring on
at least 15 days per month for a duration of three months or longer1. They
represent a debilitating neurological disorder that places a considerable
strain on the individual, ultimately diminishing their quality of life (QOL).
Compared with episodic headaches, those who suffer from chronic headaches
experience greater impairment in Health-Related Quality of Life (HRQoL), higher
rates of missed activities of daily living and frequent psychiatric
comorbidities such as anxiety and/or depression1. Acute therapies include
analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs) or
migraine-targeting therapeutics such as triptans or ergot derivatives.
Preventive treatments remain limited, with evidence supporting only a few
agents such as onabotulinumtoxinA (BoNT-A), topiramate and CGRP-targeted
monoclonal antibodies2. Despite the variety of pharmacological options,
frequent use is discouraged due to the risk of medication adverse effects or
precipitation of medication overuse headaches (MOH). This underscores the need
for non-pharmacologic adjuncts, such as osteopathic manipulation treatment
(OMT) and acupuncture.
Osteopathic manual therapy (OMT) is a form of manual therapy taught as
part of the curriculum in American Osteopathic Medical Schools and
international Osteopathy programs that emphasize the body’s natural capacity
for self-healing through the interplay of structure and function. In several
studies, OMT has been shown to effectively treat headaches by a few mechanisms,
including releasing restrictions in fascia, joints and muscles, thereby
promoting a return to physiologic homeostasis3. In parallel, studies suggest
that acupuncture is effective for a variety of chronic conditions, including
headaches, as it has few adverse effects while promoting analgesia, releasing
endogenous endorphins and improving psychological stability4. Although both OMT
and acupuncture show promise in the broader management of acute and chronic
pain as individual treatments, their roles when applied together in a cohesive
treatment model in headache treatment remain unexplored3-5. This case report
aims to describe a patient with refractory, chronic headache whose symptoms and
QOL improved following a multimodal musculoskeletal treatment approach that
incorporated OMT, acupuncture and additional therapeutic modalities.
Case Report
A 66-year-old female patient, with a past medical history significant
for squamous cell carcinoma of the scalp vertex excised in February 2024,
sought care for her persistent headaches that began in May 2024. She described
the pain as an aching sensation that originated at the base of her left occiput
and radiated anteriorly across the scalp. Her headaches occurred daily, lasted
multiple hours, but were without photophobia, phonophobia or aura. Given the
concern of new-onset headache, an MRI was performed, which revealed a 1-cm
right caudal mass (Figure 1).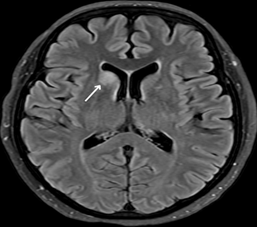
Figure
1:
Axial FLAIR MRI of the brain reveals a 1-cm hyperintense lesion in the right
caudal region (arrow)
She
was subsequently evaluated by multiple physicians, in which there were
differences in the leading differential diagnosis, including glioma, venous
angioma or nonspecific white matter disease. Neurosurgical evaluation
recommended non-surgical management and serial MRI monitoring, which revealed
unchanging size and appearance of the intracranial lesion. Despite radiographic
stability, her headaches worsened in duration and intensity, which
substantially impaired her QOL. The patient’s headaches were most likely
multifactorial in origin, with plausible contributors being the intracranial
lesion, prior vertex carcinoma excision, cervical and periscapular
musculoskeletal dysfunction, postural abnormalities and/or age-related
degenerative changes.
Initial
management, including physical therapy, dry needling, Rimegepant (Nurtec) and
NSAIDs, provided only a transient benefit. After approximately 12 months of
persistent, refractory symptoms, the patient presented to our family medicine
and lifestyle medicine clinic in May 2025 for further evaluation. On physical
examination, there were no focal neurological deficits; however,
musculoskeletal assessment revealed upper trapezius hypertonicity, weakness of
the scapular depressors and tenderness to palpation at the occipital base.
Based on her symptomatology and physical examination findings, her headaches
demonstrated features consistent with chronic cervicogenic headache and
occipital neuralgia.
A
multimodal musculoskeletal approach was used for treatment, which incorporated
acupuncture, OMT and a home exercise program. The treatment began with
acupuncture using posterior cervical and upper thoracic acupoints that
corresponded with the patient’s pain distribution (Figure 2) with the
goal of modulating nociceptive input and improving regional muscle tension.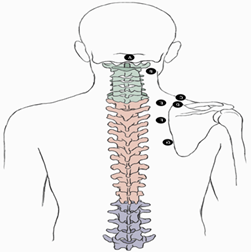
Figure
2:
Acupoints used in adjunctive therapy for headaches in the reported case
A:
GV16; B: BL10; C: GB21; D: TW15; E: BL11; F: BL13; G: BL38. Although
illustrated unilaterally, all points were applied bilaterally during treatment
Following
acupuncture, osteopathic manipulative techniques (OMT) were utilized to
optimize musculoskeletal function by addressing relevant somatic dysfunction.
Myofascial release (MFR) and then muscle energy (ME) were performed to target
trapezius hypertonicity and scapular depressor weakness. The treatment sequence
was then concluded with a high-amplitude, low-velocity (HVLA) thrust to the
thoracic spine to improve any residual thoracic restriction, restoring thoracic
mobility. Due to exhibited weakness in scapular depression, the patient was
given a daily exercise plan based on reciprocal inhibition principles to help
activate her scapular depressors, thus reducing muscular tone in upper-cross
muscles that may contribute to headaches6.
These therapies were done at her weekly appointments over the next month, with
progressive refinement based on symptomology. During her treatments, the
patient reported no adverse effects from therapy, including worsening headache
symptoms, new neurologic complaints, dizziness, syncope or functional
impairment. She was eventually seen every three weeks and by six months of
treatment, she reported substantial and sustained clinical improvement in
headache frequency and intensity, which allowed her to have less reliance on
medication and improve her sleep quality (Table 1).
Table
1:
Comparative assessment of patient’s symptoms before and after treatments at 6
month follow up
|
|
Before
treatment |
After
6 months of treatment |
|
Headache
Frequency |
Daily |
1-2
per month |
|
Headache
Duration |
At
least 4 hours |
Maximum
1-2 hours long |
|
Awakened
from sleep due to pain |
1
time/week |
No
longer occurring |
|
Severe
headache limiting daily function |
2
episodes/week |
No
longer occurring |
|
NSAID
dependency |
Four
Ibuprofen tablets daily |
Required
medication twice (two ibuprofen each) in the last six months |
Discussion
Headaches
represent one of the most common reasons for medical visits, both in emergency
and primary care settings3. The
pathophysiologic mechanism of chronic headaches is often multifactorial,
including a combination of psychological stress, lifestyle triggers,
musculoskeletal dysfunction and alterations in the central and peripheral pain
pathways. As seen in this case, conventional therapies do not always provide
sustained symptomatic relief and improvement in QOL. Since prior attempts at
management provided only transient benefit, it was clear that a broader
therapeutic approach was necessary and that no single modality was sufficient.
With that, a multimodal musculoskeletal approach was used to engage in multiple
therapeutic pathways, including biomechanical, myofascial and neuromodulator
mechanisms9. In this patient,
diagnostic evaluation could not attribute the symptoms to a single aetiology;
however, physical examination did reveal cervical and periscapular dysfunction,
which are known to contribute to cervicogenic headaches. In patients with
headache phenotypes characterized by occipital neuralgia and cervicogenic
features, such as this patient, targeted manual therapies may help alleviate
symptoms by reducing cervical and suboccipital muscle tension and improving
biomechanical function7.
Chronic
headaches and OMT
It
is important to acknowledge that the brain itself does not have pain receptors
and so the headache pain is often referred from the surrounding head, neck and
upper thoracic structures. Specifically, the muscles of the suboccipital
triangle, rectus capitis posterior major and obliquus capitis superior and
inferior can undergo hypertrophy and/or asymmetry, resulting in possible
occipital nerve compression. Dysfunctions in these musculoskeletal structures
can perpetuate symptoms, which underscores the potential value of osteopathic
manipulation in targeting these dysfunctions. In many cases, dysfunctions in
the body can manifest as observable TART changes, also known as viscero-somatic
dysfunctions. TART is an osteopathic acronym that refers to tissue texture
changes, asymmetry, restricted motion and tenderness8. It is through these palpable changes, as
well as other physical examination findings, that a somatic dysfunction can be
diagnosed. OMT is not only used to diagnose somatic dysfunctions, but can also
provide treatment by alleviating symptoms and subsequently reducing pain3. Generally, treatments can be categorized
as either active or passive (based on the patient’s involvement) and direct or
indirect (based on the direction of treatment being away from or towards the
restriction)8. The most common
osteopathic techniques in the cervical spine are myofascial release and muscle
energy8.
In
terms of the utilized treatment for this patient, myofascial release was
applied in both a direct and indirect technique, with passive movements
following the fascia in all directions of ease. This is intended to release the
tension in the fascia and muscle fibres of the hypertonic upper-cross and
cervical muscles. Both post-isometric relaxation and reciprocal inhibition of
muscle energy were utilized in the patient’s treatment plan. Muscle energy with
post-isometric relaxation involved contracting the upper trapezius and
rhomboids against an isometric force by the physician, followed by a few
seconds of relaxation, which allowed for lengthening of the hypertonic muscles
and increasing range of motion9.
The treatment ended with HVLA, which was an applied, rapid force directed at
the cervical facet joints, engaging the restrictive barrier and ultimately
releasing the restriction9. Beyond
in-office manual intervention, multimodal care also focuses on addressing
psychosocial and lifestyle factors, including postural habits5. Postural habits, including forward-head
posture and chronically elevated scapular positioning, can lead to inhibition
and poor neuromuscular control of key scapular stabilizers. With weakened
scapular stabilizers, there is compensatory overuse of upper-cross and cervical
muscles and subsequently increased tension in the cervicothoracic junction10. Reducing hypertonic muscles like the
rhomboids helps restore proper scapular motion and positioning, thereby
reducing the mechanical stress that contributes to headache triggers. As seen
in this case, this was ensured by providing the patient with a home exercise
plan grounded in the principles of reciprocal inhibition and emphasizing
posterior scapular chain activation6.
The patient was instructed to perform an activation drill emphasizing
controlled scapular retraction followed by scapular depression to
preferentially activate antagonist muscles, like the lower trapezius and
pectoralis minor. Activation of the stretch reflex of the muscle spindle fibres
of those muscles caused the agonist muscles, such as the upper trapezius and
rhomboids, to reflexively relax9.
Additionally, this activation drill simultaneously retrained scapular control
away from a chronically elevated posture towards a more dynamic motion.
Researchers
hypothesize that OMT rebalances the autonomic nervous system, reduces
pro-inflammatory substances, activates Golgi tendon organs and inhibits
hypertonic muscles, all of which are associated with headaches3,7. Multiple systematic reviews and
clinical trials have demonstrated that OMT significantly reduces pain intensity
and improves function in patients with chronic musculoskeletal pain, such as
chronic back pain. Specifically in headaches, OMT has been associated with
reductions in headache frequency, intensity and duration, as well as
improvement in functional outcomes and QOL8.
Not only do osteopathic techniques reduce pain, but studies have also indicated
that combining multiple osteopathic approaches yields greater relief and
headache reduction7.
OMT
has demonstrated a favourable safety profile, with reported adverse effects of
discomfort, light-headedness and/or stiffness. Most of these adverse effects
were reported within four hours of treatment and almost 75% had resolved
symptoms within 24 hours11. In
addition to safety, evidence suggests potential downstream benefits of manual
therapies in reducing medication reliance. A large retrospective cohort study
of adults with tension-type headache found that patients receiving spinal
manipulative therapy had a significantly lower risk of butalbital prescription
and a reduced risk of developing medication overuse headache over two years of
follow-up compared with matched controls12.
Although current evidence supports OMT as a low-risk modality, additional
studies with larger sample sizes are needed to fully characterize the safety
and long-term outcomes of OMT, particularly when multiple techniques are
applied in a single session11,12.
Chronic
headaches and acupuncture
Recent
studies, in parallel with Western medicine, have shown that acupuncture may
stimulate the release of endogenous opioids, serotonin and norepinephrine that
have downstream effects on nociceptors, inflammatory cytokines and
physiological pain perception13.
However, the mechanism of acupuncture is not completely known13. Chronic headaches involve dysfunctional
pain processing and central sensitization, including altered activity within
brainstem pain modulatory circuits and trigeminovascular pathways2. These neurological pathways may be
influenced by the neuromodulator effects proposed in acupuncture therapy,
providing a plausible contribution for symptom modulation in refractory
headaches. Acupuncture has been studied explicitly in patients with chronic
headaches, in which a Cochrane review showed that patients who received verum
acupuncture had at least a 50% reduction in headache frequency when compared
with usual care or sham acupuncture13.
Additionally, another study showed that acupuncture improved the general state
of health, mental health and functional capacity domains4. Ultimately, the authors concluded that
acupuncture reduced pain and frequency of crises, minimized dependence on
analgesics, improved quality of life and recommended it as an adjunctive
therapy for those suffering from chronic headaches4,13.
Regarding
safety, both acupuncture and OMT are generally regarded as low-risk treatment
options. Acupuncture is generally well tolerated, with minimal adverse effects,
such as fatigue, local pain or micro bleeding14.
With any procedure that involves needle introduction, there is a risk of
bleeding, infection, nerve injury or trauma, such as a pneumothorax14. Overall, complications with acupuncture
are infrequent and result in far fewer adverse effects relative to
pharmacological therapies14.
However, additional clinical studies are needed to further assess the safety of
acupuncture in the treatment of headache disorders13,14.
In
addition to its safety profile, it is relatively cost-effective compared to
standard care. For example, economic analyses from the United Kingdom estimated
a cost of $12,080 per quality-adjusted-life-year (QALY) gained with acupuncture
for patients suffering from chronic headache disorders, which falls well below
commonly accepted cost-effectiveness thresholds13.
By comparison, long-term pharmacologic management may offer limited sustained
benefit, is associated with potential adverse effects and may be associated
with higher long-term cost depending on medication class and duration of use5. Overall, available evidence supports
acupuncture as a safe and cost-effective therapeutic option for the management
of chronic headache disorders.
Multimodal
musculoskeletal model
Acupuncture
and OMT have gained increasing recognition for their effectiveness in disorders
resulting in chronic pain3,13.
Not only do both independently serve as effective treatments for pain, but when
applied as a multimodal musculoskeletal treatment model, they can produce
synergistic and lasting benefits5.
Although individual therapies have been shown to reduce headache burden,
studies have shown that a multimodal musculoskeletal treatment approach
optimizes pain management and rehabilitation5.
Pain is inherently complex and multifactorial. It is shaped by biological,
psychological and lifestyle factors. Therefore, a more holistic approach is
necessary to address all dimensions associated with pain management.
Integrating multiple therapeutic modalities allows healthcare providers to
address the physical, psychological and functional symptoms by leveraging the
strengths of each modality. Unfortunately, current musculoskeletal care is
often fragmented in practice. Patients are being referred to multiple providers
for the management of a single clinical issue, which delays care and reduces
follow-through. This delay causes many to rely solely on pharmacological
measures5. This fragmentation is
linked to prolonged pain, decreased function and poorer outcomes. However, a
coordinated, multimodal approach can improve the level of care integration,
promoting continuity of care. Providers can deliver this coordinated care
either through a single practitioner skilled in multiple therapies or within a
clinic where all services are accessible in the same facility in conjunction
with one another5. This approach
is particularly valuable for chronic headaches, many of which either arise from
or are exacerbated by musculoskeletal dysfunction. Even in secondary headaches
not caused by musculoskeletal dysfunctions, postural strain and muscle tension
can still develop, further worsening symptoms. Addressing these musculoskeletal
dysfunctions in an integrated way can help break the pain cycle and improve
overall outcomes. In this case, the precise cause of the patient’s headaches
was uncertain. Despite this uncertainty, she experienced significant symptom
relief and improved function. This case highlights the value of multimodal care
in providing meaningful benefits for patients with chronic headaches, even when
the underlying pathology is unclear.
Limitations
Certain
limitations should be considered when interpreting this case. After initial
imaging revealed a 1-cm caudal mass, serial MRIs were performed. However, the
mass remained unchanged in terms of size and appearance and subsequently was
unable to be used to monitor the patient’s symptoms and/or response to
treatment. Instead, treatment response was primarily measured using symptom
outcomes reported by the patient, including headache frequency, intensity,
duration, sleep disruption, functional limitation and medication use. Given the
potential for bias, future studies should include the use of a standardized,
objective metric separate from subjective data. As this report involved a
single individual, future studies should include larger sample sizes and control
groups to enhance generalizability and strengthen the evidence. In this
patient, there were multiple contributors that could have led to her headache,
such as the stable intracranial lesion, post-surgical changes, musculoskeletal
dysfunction, postural strain and age-related degenerative changes. Therefore,
the observed improvement in symptoms cannot be attributed to the treatment of a
single headache subtype. Additionally, further investigation is warranted to
determine whether combined multimodal therapies is superior in terms of
clinical benefit in comparison to individual interventions alone. All of these
future studies will help further establish the efficacy of both OMT and
acupuncture as individual interventions in chronic headaches, as well as when
used in combination.
Conclusion
Patients
with persistent, chronic headaches frequently experience debilitating physical,
psychological and functional impairment, which can significantly impact a
patient's quality of life. In this report, a coordinated multimodal
musculoskeletal treatment approach was used in the management of a patient
suffering from chronic headaches resistant to conventional care. This treatment
plan integrated OMT, acupuncture and home exercises, all rendered by a single
physician provider. Following this intervention, the patient reported reduced
headache frequency and intensity, improved sleep quality, decreased reliance on
analgesic medications and enhanced ability to perform activities of daily
living. While these findings are limited by the descriptive nature of a single
case, this report supports consideration of a coordinated, patient-centred,
multimodal approach for chronic headaches that are refractory to conventional
management. The observed clinical improvement reflects that the combination of
multiple therapeutic modalities may have a synergistic effect. It has been in
both the authors’ clinical experience in this current case, as well as other
cases, that the combination of multiple interventions at once provided improved
clinical outcomes. Due to the significant global impact of headaches, further
investigation, using larger cohorts and standardized outcome scales, is
warranted to determine whether multimodal musculoskeletal interventions are
clinically superior to individual therapies.
Acknowledgements
No
additional acknowledgements to declare.
Conflicts
of interests
No
conflicts of interest to declare.
Funding
No
funding to declare.
Ethical
Approval
Consent
of all participants was obtained.
References
1. Ahmed F, Parthasarathy R, Khalil M. Chronic daily headaches. Ann
Indian Acad Neurol 2012;15:40-50.
2. Mungoven TJ, Henderson
LA, Meylakh N. Chronic Migraine Pathophysiology and Treatment: A Review of
Current Perspectives. Frontiers in Pain Res 2021;2.
3. Chin J, Qiu W, Lomiguen CM, Volokitin M.
Osteopathic Manipulative Treatment in Tension Headaches. Cureus 2020;12(12)
4. Mayrink WC, Garcia JBS, Dos
Santos AM, Nunes JKVRS, Mendonça THN. Effectiveness of Acupuncture as Auxiliary
Treatment for Chronic Headache. J Acupuncture Meridian Studies
2018;11(5):296-302.
5. Behringer C, Nagib N,
Nagib N. Introduction to multimodal musculoskeletal treatment models: a
viewpoint. Discover Applied Sciences 2025;7(8).
6. Owensboro Health.
Posterior Chain Activation 2. YouTube 2026.
7. Jara Silva CE, Joseph AM,
Khatib M, et al. Osteopathic Manipulative Treatment and the Management of
Headaches: A Scoping Review. Cureus 2022;14(8).
8. Lumley H, Omonullaeva N,
Dainty P, Paquette J, Stensland J, Reindel K. Current Use and Effects of
Osteopathic Manipulative Treatment (OMT) in the Military: A Scoping Review.
Cureus 2025.
9. Roberts A, Harris K,
Outen B, et al. Osteopathic Manipulative Medicine: A Brief Review of the
Hands-On Treatment Approaches and Their Therapeutic Uses. Medicines.
2022;9(5):33.
10. Im B, Kim Y, Chung Y, Hwang
S. Effects of scapular stabilization exercise on neck posture and muscle
activation in individuals with neck pain and forward head posture. J Physical
Therapy Sci 2015;28(3):951-955.
11. Degenhardt BF, Johnson JC,
Brooks WJ, Norman L. Characterizing Adverse Events Reported Immediately After
Osteopathic Manipulative Treatment. J American Osteopathic Association
2018;118(3):141.
12. Trager RJ, Williamson TJ,
Makineni PS, Morris LH. Association Between Spinal Manipulation, Butalbital
Prescription and Medication Overuse Headache in Adults with Tension‐Type
Headache: Retrospective Cohort Study. Health Science Reports 2024;7(12).
13. Kelly RB, Willis J.
Acupuncture for Pain. American Family Physician 2019;100(2):89-96.
14. Van Hal M, Dydyk AM, Green
MS. Acupuncture. PubMed 2023.