Primary Intra-Thoracic Evans Tumor in A Young Female: Case Report and Literature Review
Abstract
Evans tumor, also known as low-grade fibromyxoid sarcoma, usually
presents as a slowly growing, painless mass in young adults, most commonly
involving the proximal extremities. Involvement of the intrathoracic
compartment has been rarely described, most often as a site of metastasis.
Primary intrathoracic low-grade fibromyxoid sarcoma of the pleura is even
rarer. Here, we describe a case report of a young lady with a history of
psoriatic arthritis who initially presented with shortness of breath due to left
pleural effusion. Further workup revealed a primary intrathoracic low-grade
fibromyxoid sarcoma of the left pleura.
Keywords: Evans
tumor; Fibromyxoid sarcoma; Intrathoracic compartment; Metastasis; Left pleura
Introduction
Low-grade fibromyxoid sarcoma (LGFMS) was first
described in 1987 by American pathologist Harry L. Evans and hence, it is also
known as Evans tumor. As the name suggests, this tumor is an admixture of
cellular myxoid zones and collagenous zones interspersed with bland spindle
cells in a whorling or storiform pattern. It is relatively rare and even rarer
is when it presents as a primary intrathoracic tumor. Here, we report a case of
a primary intrathoracic Evans tumor in a young female.
Case report
A
37-year-old female with a medical history of psoriatic arthritis (on
Ixekizumab) presented to the emergency room with gradual onset dyspnea, easy
fatigability and central chest pain, progressively worsening over the last two
months. She was a former smoker (2 pack years, quit at age 22) with no major
exposures. Admission chest radiograph revealed left-sided pleural effusion, for
which thoracentesis was performed, obtaining 800cc of straw-colored fluid. It
was transudative by Light's criteria and cytology was consistent with benign
mesothelial cells. Further workup included a CT scan of the chest, abdomen and
pelvis, which revealed multiple enhancing pleural-based masses involving the
left hemithorax (Figure 1).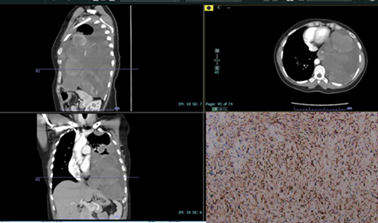
Figure
1:
CT Chest in sagittal (upper left), axial (upper right) and coronal views
(bottom left) showing a large loculated left pleural effusion containing
multiple enhancing pleural-based masses. This is an ill-defined, partially
calcified 8.9 x 5.8 cm pleural-based mass (red arrow) and a homogeneously
enhancing mass more superiorly (blue arrow) in the pleural space measuring 8.8
x 5.8 cm were noted. Numerous additional morphologically similar masses are
present involving the left mediastinal, costal and diaphragmatic pleural
surfaces (green arrow). The bottom right image shows strong MUC 4 positive
staining (black arrow) on the biopsy specimen, confirming low-grade fibromyxoid
sarcoma.
There
was no evidence of malignancy in the abdomen or pelvis. Incidentally, serum
tumor marker CA125 was elevated. A PET scan revealed mild to moderate FDG-avid
left-sided pleural-based masses with calcifications predominantly involving the
inferior left hemithorax.
Since
the percutaneous ultrasound-guided biopsy was inconclusive and the bronchoscopy
was unremarkable, an exploratory left thoracoscopy with biopsy was performed,
which revealed multiple pleural-based nodules. The histological specimen
consisted of bland spindle cells in a loose myxomatous stroma. Immunostaining
was negative for pancytokeratin, CAM5.2, calretinin and CD34, but positive for
MUC4 (Figure 1). A diagnosis of
primary intrathoracic low-grade fibromyxoid sarcoma was made and
immunochemotherapy (Trabectedin/Ipilimumab/Nivolumab) was initiated. Follow up
in 6 months documented the stability of the tumour, with no recurrence.
Discussion
Low-grade
fibromyxoid sarcoma (also known as Evans tumor) usually appears as a slowly
growing, painless mass predominantly in young adults, with a median age of 34
years and a range from 3 to 78 years1,2.
The most reported site is the proximal extremities, particularly the thigh or
trunk originating in the deeper soft tissue layers. Rarely, these tumors have
also been found in the viscera, retroperitoneum and intrathoracic compartments,
either as a metastatic process or as a primary tumor3. These tumors can grow up to 23 cm. The
clinical presentation of this tumor varies and can range from gradually
progressing respiratory symptoms to a large pleural effusion.
Radiologically,
the tumor appears as a multinodular mass with alternating strong
(hypercellular) and weak (myxoid) enhancing areas featuring abrupt transitions5,6. Ultrasound and MRI findings have also
been described7,8. Diagnosis is
usually made through histology and immunostaining of the tumor after resection.
Histologically,
this tumor appears as hyalinizing spindle cells with giant rosettes and
fibromyxoid zones. The spindle cells have distinct cytoplasm with a near
absence of mitotic figures, hence referred to as “low grade." The fibrous
areas have abundant stromal collagen, either as rosettes or with whorled
patterns of growth9,10.
Immunostaining
is typically negative for S100, desmin, keratin, pan-cytokeratin, CAM 5.2,
calretinin and CD34 and positive for MUC4. LGFMS characteristically expresses
the FUS-CREB3L2 fusion (t7;16:q32-34;p11) by RT-PCR9,11.
Treatment
includes excision of the tumor, metastasectomy, radiation and
chemoimmunotherapy (trabectedin, ipilimumab, nivolumab)2,9,11-14.
This
tumor may exhibit a progressive course with high rates (6% to 64%) of
recurrence (up to 15 years) and metastasis (up to 45 years), showing a “low
grade” appearance on histology4,15.
Although histological appearance should not be used for prognostication, a
“de-differentiated recurrence” with anaplastic round cell morphology may
indicate short survival. Therefore, it may be necessary to closely follow up
with imaging surveillance for a long term after excision16.
Conclusion
This is a rare case of primary intra-thoracic
low-grade fibromyxoid sarcoma in a young female, presenting as pleural based
masses. Percutaneous biopsy may be inconclusive and thoracoscopic biopsy may
eventually be required. Immunostaining will help in confirming the diagnosis.
The treatment involves a combination of surgery, radiation and
chemoimmunotherapy.
References
2. Cowan ML, Thompson LD, Leon ME, et al. Low-Grade Fibromyxoid Sarcoma of the Head and Neck: A Clinicopathologic Series and Review of the Literature. Head and Neck Pathol 2016;10:161-166.
3. Porrino J, Al-Dasuqi K, Irshaid L, et al. Update of pediatric soft tissue tumors with review of conventional MRI appearance-part 1: tumor-like lesions, adipocytic tumors, fibroblastic and myofibroblastic tumors and perivascular tumors. Skeletal Radiol 2022;51:477-504.
4. Evans Harry L. MD. Low-Grade Fibromyxoid Sarcoma: A Clinicopathologic Study of 33 Cases with Long-Term Follow-Up. The American J Surg Pathology 2011;35(10):1450-1462.
5. Sargar K, Kao SC, Spunt SL, Hawkins DS, Parham DM, Coffin C, Mc Carville MB. MRI and CT of Low-Grade Fibromyxoid Sarcoma in Children: A Report from Children's Oncology Group Study ARST0332. AJR Am J Roentgenol 2015;205(2):414-420.
6. Maeda E, Ohta S, Watadani T, et al. Imaging findings of thoracic low-grade fibromyxoid sarcoma: report of three cases. Jpn J Radiol 2009;27:375.
7. Koh SH, Choe HS, Lee I, et al. Low-grade fibromyxoid sarcoma: ultrasound and magnetic resonance findings in two cases. Skeletal Radiol 2005;34:550-554.
8. Kim SY, Kim MY, Hwang YJ, et al. Low-grade fibromyxoid sarcoma: CT, sonography and MR findings in 3 cases. J Thorac Imaging 2005;20(4):294-297.
9. Mustafa S, VandenBussche CJ, Ali SZ, Siddiqui MT, Wakely PE Jr. Cytomorphologic findings of low-grade fibromyxoid sarcoma. J Am Soc Cytopathol 2020;9(3):191-201.
10. Murshed KA, Al-Bozom I, Ammar A. Sclerosing epithelioid fibrosarcoma: in-depth review of a genetically heterogeneous tumor. APMIS 2021;129(8):455-460.
11. Martínez-Trufero J, Cruz Jurado J, Gómez-Mateo MC, et al. Uncommon and peculiar soft tissue sarcomas: Multidisciplinary review and practical recommendations for diagnosis and treatment. Spanish group for Sarcoma research (GEIS - GROUP). Part I. Cancer Treat Rev 2021;99:102259.
12. Sajid MI, Arshad S, Abdul-Ghafar J, Fatimi SH, Din NU. Low-grade fibromyxoid sarcoma incidentally discovered as an asymptomatic mediastinal mass: a case report and review of the literature. J Med Case Rep 2021;15(1):50.
13. Demetri GD, von Mehren M, Jones RL, et al. Efficacy and Safety of Trabectedin or Dacarbazine for Metastatic Liposarcoma or Leiomyosarcoma After Failure of Conventional Chemotherapy: Results of a Phase III Randomized Multicenter Clinical Trial. J Clin Oncol 2016;34(8):786-793.
14. D'Angelo SP, Mahoney MR, Van Tine BA, et al. Nivolumab with or without ipilimumab treatment for metastatic sarcoma (Alliance A091401): two open-label, non-comparatives, randomized, phase 2 trials. Lancet Oncol 2018;19(3):416-426.
15. Saab-Chalhoub MW, Al-Rohil RN. Low-grade fibromyxoid sarcoma of acral sites: Case report and literature review. J Cutan Pathol 2019;46:271-276.
16. Folpe AL, Lane KL, Paull G, Weiss SW. Low-grade fibromyxoid sarcoma and hyalinizing spindle cell tumor with giant rosettes: A Clinicopathologic study of 73 cases supporting their identity and assessing the impact of high-grade areas. Am J Surg Pathol 2000;24(10):1353-1360.