Pyogenic Granuloma of the Vocal Cords: A Rare Benign Lesion Mimicking Malignancy
Abstract
The pyogenic granuloma (or botryomycoma) of the vocal
cords is a rare benign tumor. It is typicallylocated in the posterior part,
near the vocal process of the arytenoid cartilage. Etiologies
includegastroesophageal refl ux, intubation and vocal strain.
Macroscopically, laryngoscopic examination usually
reveals a nodular lesion; however, it may alsopresent as an ulceration of the
vocal cord. Its appearance can therefore be misleading, resembling amalignant
laryngeal lesion, with the diagnosis confi rmed by histopathological
examination.
Histologically, a pyogenic granuloma is not a true
granuloma. It is rather a reactive process,characterized by the presence of
intact or ulcerated squamous epithelium overlying granulation tissue orfi
brosis.
Treatment primarily involves surgical excision of the
lesion, under direct laryngoscopy, coupled withmanagement of gastroesophageal
refl ux, which may be silent. Despite its benign nature, pyogenicgranuloma has
a potential for recurrence, especially if the underlying cause persists.
Keywords: Pyogenic granuloma; Botryomycoma; Vocal cords; Dysphonia;
Gastroesophageal reflux; Intubation; Benign laryngeal tumor
Introduction
Lesions of the glottic region, which primarily
present as dysphonia, encompass a wide spectrum of pathologies with varying
degrees of malignancy. These range from inflammatory conditions and benign
lesions such as vocal cord nodules and polyps to malignant neoplasms.
Management depends on the exact nature of the lesion and its underlying cause.
Vocal process granuloma, also known as pyogenic
granuloma, is a benign lesion that can none the less raise clinical suspicion
due to its presentation, which may resemble laryngeal cancer. Synonyms for this
lesion include contact ulcer, intubation granuloma, vocal granuloma or
inflammatory polyp of the larynx. A thorough clinical evaluation is therefore
essential to differentiate this benign condition from malignant lesions and
provide appropriate management.
Case Presentation
A
58-year-old patient presented with a one-year history of dysphonia. His medical
history included a smoking habit of 7 pack-years, stopped over 30 years ago,
type 2 diabetes, hypertension and basal cell carcinoma (BCC) of the nasal tip.
The BCC required six surgical interventions, including re-excisions for
inadequate tumor margins and reconstruction procedures, each involving
orotracheal intubation.
The
reported dysphonia, present for a year, had worsened 15 days before
consultation. No history of vocal strain was noted. The patient also described
persistent respiratory discomfort due to nasal obstruction but denied dysphagia
or pharyngeal pain.
Endoscopic
examination of the vocal cords using a 70-degree rigid scope revealed a
reddish, exophytic nodular lesion occupying the posterior glottic region,
leaving only an anterior glottic gap. Vocal cord mobility was preserved.
Cervical-thoracic
CT scan revealed a glottic lesion lateralized to the right, extending to the overlying
ventricular band without proglottic space invasion. No abnormalities of the
laryngeal cartilages were noted.
The
patient underwent surgical management with complete tumor excision during
direct laryngoscopy in suspension.
Histological
examination identified polypoid fragments corresponding to polymorphic
granulation tissue with numerous engorged capillary-sized vessels arranged in
lobules. These vessels had thin walls lined by regular endothelial cells. No
evidence of malignancy was observed, concluding the diagnosis of pyogenic
granuloma of the vocal cords (Figure 1).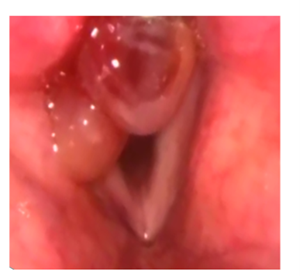
Figure
1: Polypoid lesion occupying the posterior part of the vocal cord
Discussion
Pyogenic granuloma (PG) of the vocal cords,
although rare, constitutes a benign pathology that can be misinterpreted as
malignant due to its clinical and endoscopic presentation. In our case, the
lesion’s development was likely influenced by a combination of repeated
orotracheal intubations during multiple surgeries for basal cell carcinoma
(BCC) and a possible component of silent gastroesophageal reflux, which is a
well-documented etiological factor.
The laryngoscope appearance of PG-a reddish,
exophytic nodular lesion localized to the vocal process-is suggestive but not
specific. As highlighted in the literature, these lesions may also present as
ulcerations or masses, which can affect one or both vocal cords and, in rare
cases, extend to other laryngeal regions1,2.
Consequently, histological analysis is essential for an accurate diagnosis, confirming
the presence of richly vascularized granulation tissue organized in lobules
with endothelial cell-lined vessels, while ruling out malignancy.
PG is most commonly observed in the gingiva,
lips and facial regions, with rare occurrences in the larynx. A review
conducted at the University of Virginia Medical Centre and Martha Jefferson
Hospital analyzed 639 vascular lesions of the oral cavity and upper airway.
Among these, 73 cases (11% of whichoccurred during pregnancy) were diagnosed as
PG, primarily affecting the lips (38%), nose (29%) oral mucosa (18%) and tongue
(15%). Notably, none of the laryngeal or tracheal lesions initially resembled PG
on microscopic examination3.
Andrea et al. reported a rare case of laryngeal
PG in a 23-year-old pregnant woman presenting with hemoptysis. Excision of the
lesion after delivery revealed characteristic lobular proliferation of closely packed
capillaries in an oedematous stroma4.
Similarly, Arkadi et al. described a 12-year-old girl with hemoptysis caused by
an exophytic, multilocular reddish mass nearly obstructing the hypopharynx and covering
the laryngeal inlet. Histological examination ultimately confirmed PG,
highlighting the importance of pathology in differentiating this benign
condition from other vascular or malignant lesions5.
Further, in a study by Epivatianos, et al., PG
was documented as a lobular capillary haemangioma of the oral cavity,
supporting its benign nature but emphasizing the potential for misdiagnosis due
to its appearance6. Cawson, et
al. highlighted that hormonal influences, particularly during pregnancy, could exacerbate
the presentation of PG in areas like the oral cavity and upper respiratory
tract7.
Surgical excision remains the mainstay of
treatment for PG, as demonstrated in our patient. However, addressing
underlying etiological factors, such as silent gastroesophageal reflux, is
crucial to minimizing recurrence risk. A multidisciplinary approach-encompassing
otolaryngologists, gastroenterologists and potentially speech therapists-may be
required to ensure comprehensive management and optimal outcomes.
This case underscores the critical importance
of a systematic approach to persistent dysphonia, a common yet often overlooked
symptom, necessitating vigilance for potential malignancy-mimicking lesions.
While PG is a benign entity, delayed or inappropriate treatment can lead to
complications or recurrence. Moreover, this report highlights the indispensable
role of endoscopic exploration and imaging in evaluating lesion extent, guiding
surgical intervention and optimizing postoperative follow-up.
Conclusion
Pyogenic granuloma of the vocal cords is a rare
benign lesion but can be challenging due to its clinical presentation mimicking
malignancy. This case highlights the importance of a thorough diagnostic
approach combining endoscopy, imaging and histopathological examination to
establish an accurate diagnosis and rule out malignancy. Identifying and
managing underlying etiological factors, such as gastroesophageal reflux or
laryngeal trauma, is essential to prevent recurrence. Multidisciplinary care
remains the key to optimal management and follow-up.
Declarations
The author confirms that patient consent for
publication of this case report was received.
References
1. Shah M, Feldman M, Patel A. Pyogenic granuloma of the
larynx: A rare presentation mimicking malignancy. Laryngoscope
2019;129(7):1526-1530.
5. Arkadi L, Smith T, Rhodes A. Massive pyogenic
granuloma of the larynx in a pediatric patient: A rare presentation. J Pediatr
Otorhinolaryngol 2020;138:110354.